How fast can you learn medical billing?
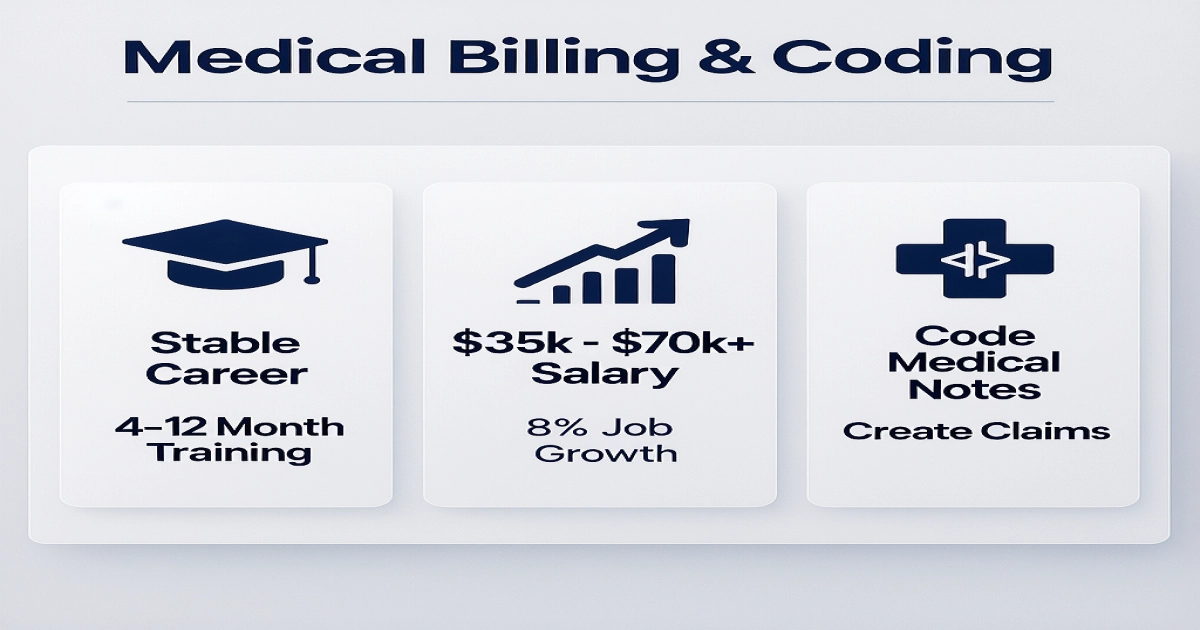
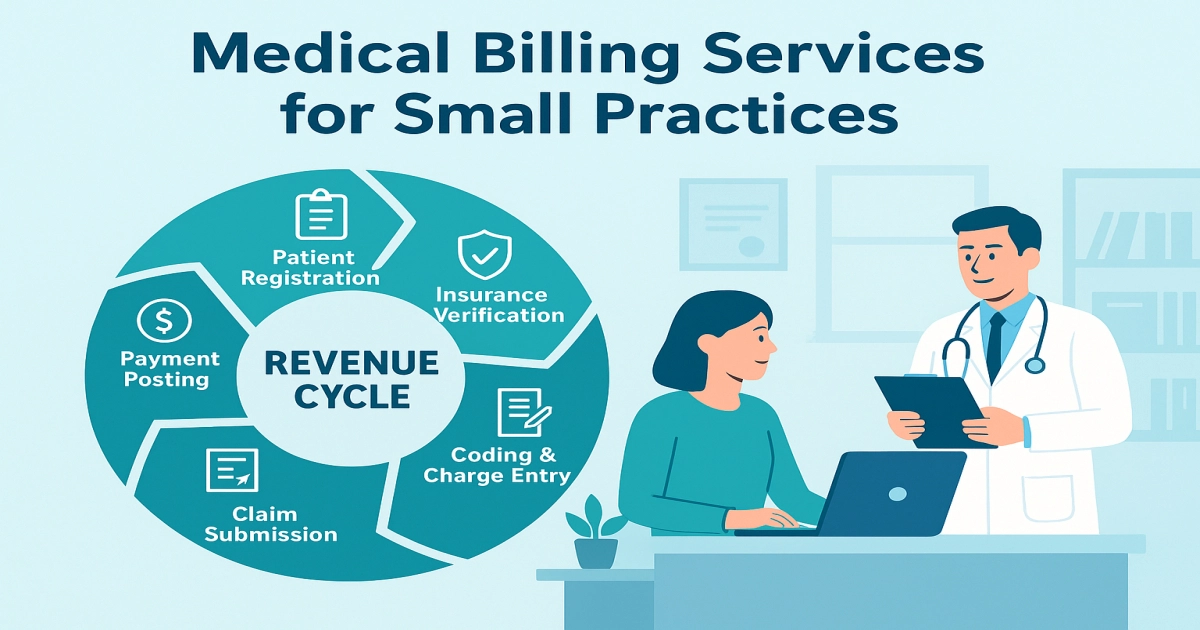
Medical billing and coding is a stable healthcare career that takes 4-12 months to learn. It involves two skills: coding doctor’s notes into universal codes and using those codes to create claims. The US healthcare system needs these professionals, with demand growing 7-8% through 2026. You can learn through a certificate, diploma, or associate degree. … Read more