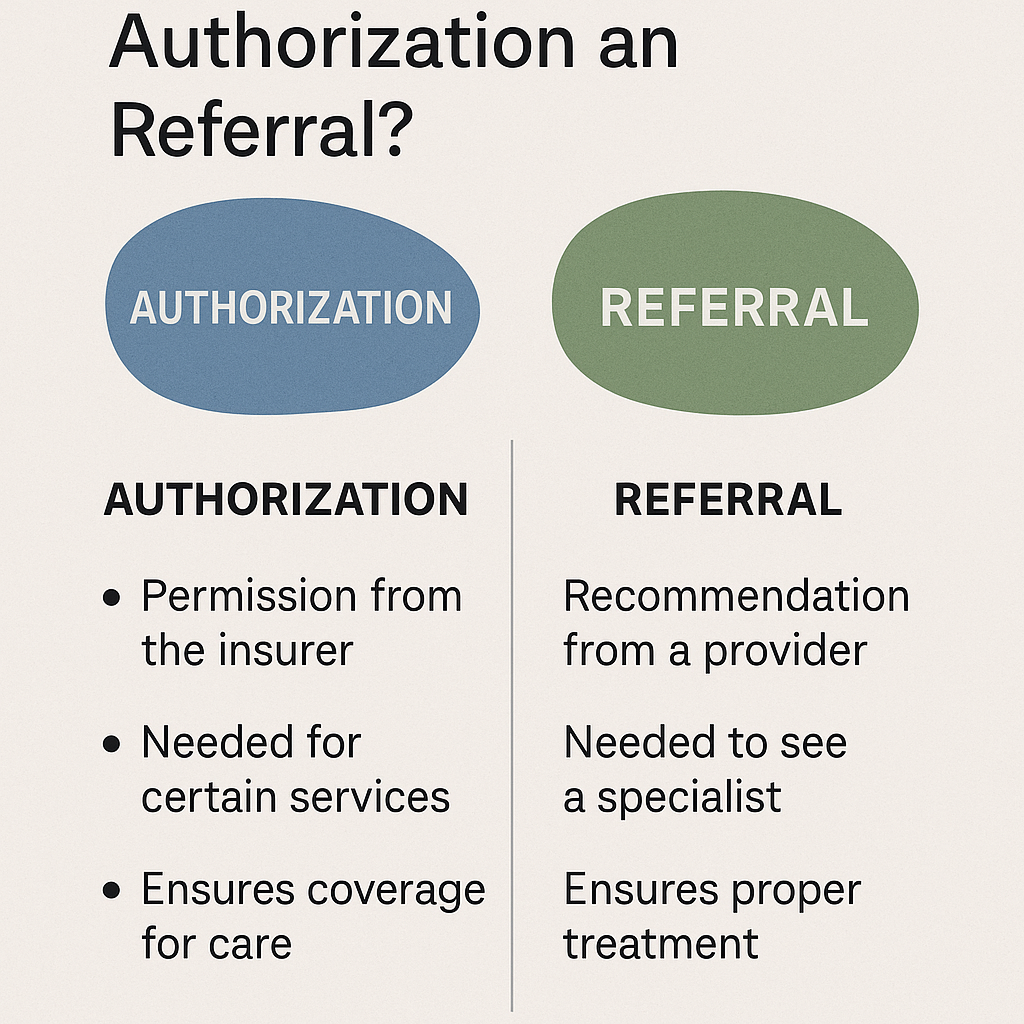
What’s the difference between authorization and referral?
In medical billing, authorization and referral serve different purposes, though both are crucial for insurance coverage and patient care. Simply put, authorization is permission from the insurance company for a service, while a referral is a recommendation from a primary care provider (PCP) to see a specialist. Let’s break down the details to help you … Read more