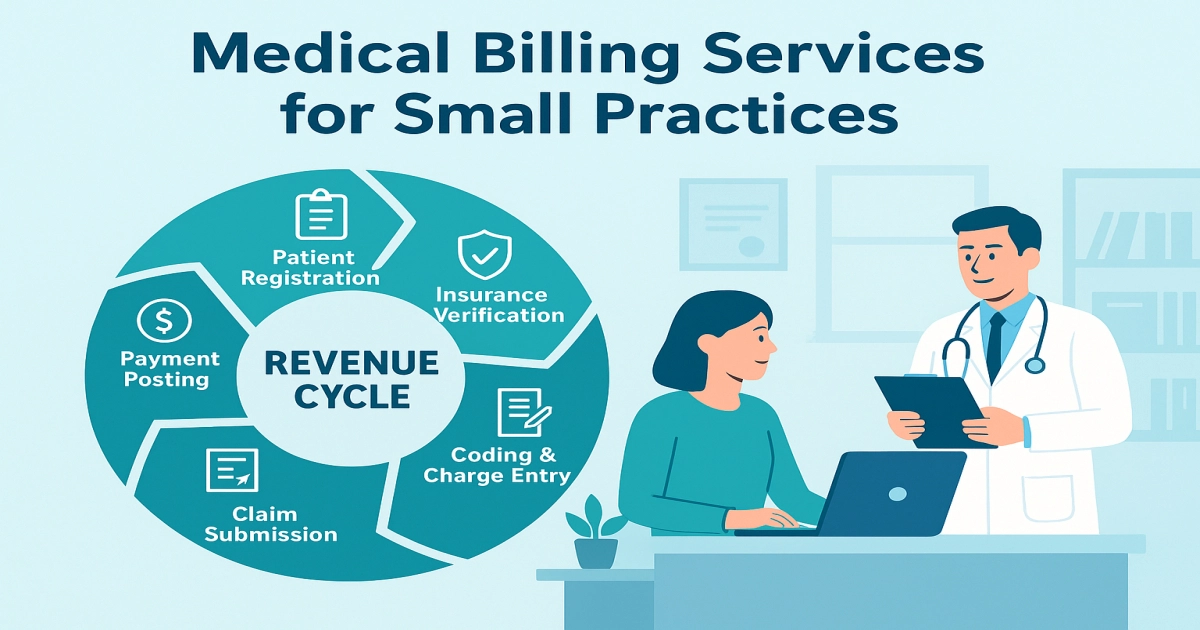
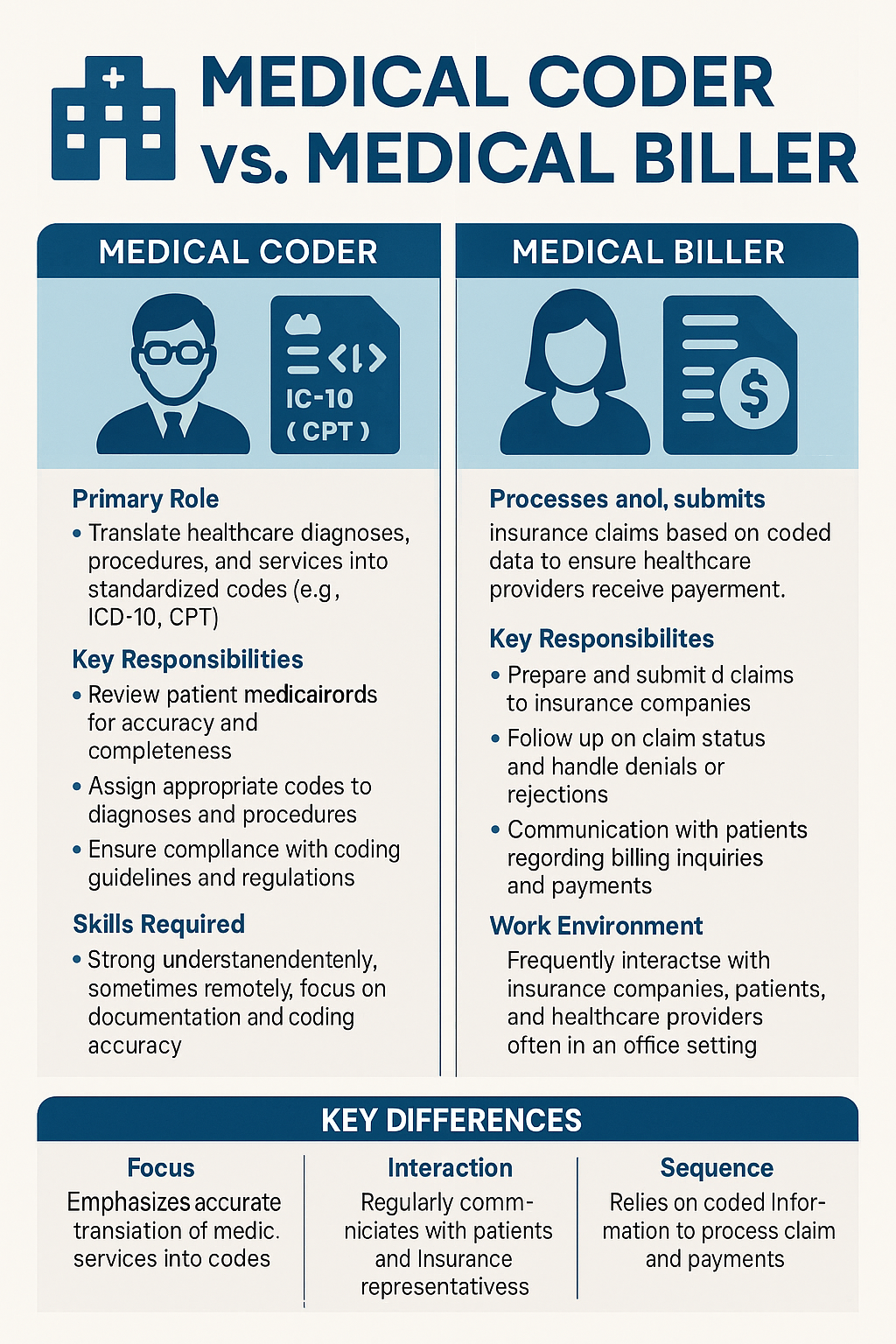
Medical Billing Services for Small Practices: Stop Losing Revenue to Claim Errors
Medical billing services for small practices handle claim submission, denial management, patient billing, and revenue cycle optimization for practices with 1-10 providers who cannot afford full-time billing staff. These services cost 4-8% of collections and typically increase revenue by 10-25% within six months by reducing claim denials, accelerating payment cycles, and eliminating billing errors that … Read more