Definition
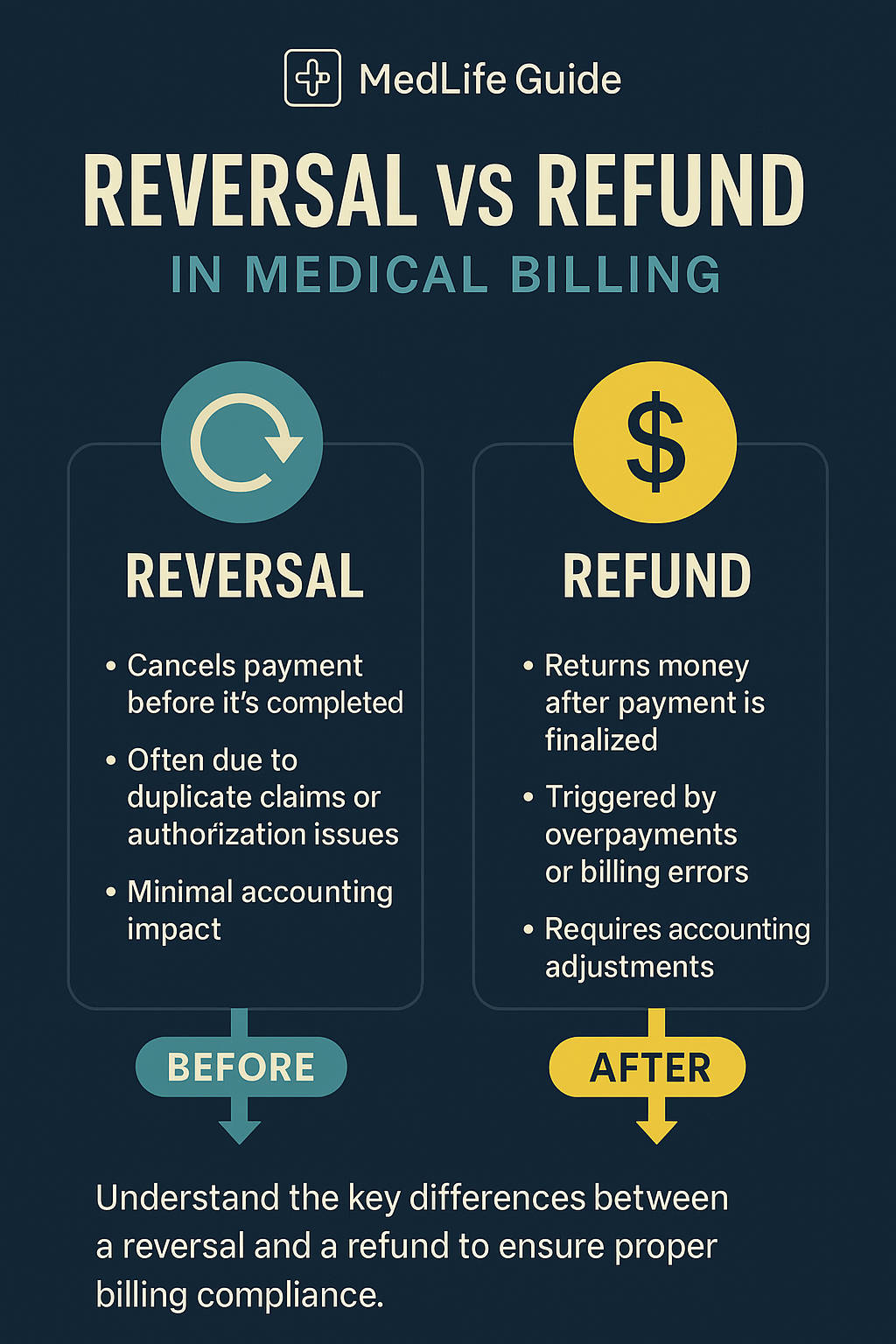
- A reversal cancels a payment before it’s completed.
- A refund returns money after a payment has been finalized.
- Knowing the difference improves accuracy, accounting records, and patient trust.
Understanding Reversals in Medical Billing
- Happens before the payment is fully processed.
- Common reasons include:
- Duplicate claims
- Incorrect patient details
- Change in authorization
- Protects accounts receivable and prevents unnecessary adjustments.
- Quick action reduces financial errors and saves time.
Understanding Refunds in Medical Billing
- Happens after the payment is finalized.
- Triggered by:
- Overpayments
- Billing errors
- Canceled or partially rendered services
- Requires formal processes, including possible appeals and adjustments.
- Affects financial audits and long-term accounting accuracy.
Quick Comparison: Reversal vs. Refund
| Aspect | Reversal | Refund |
|---|---|---|
| Timing | Before payment settles | After payment is finalized |
| Purpose | Cancel wrong/unauthorized charges | Return overpayment or correct billing errors |
| Impact on Accounting | Minimal correction needed | Requires adjustments and audit trails |
| Common Triggers | Duplicates, wrong authorization | Overbilling, service changes |
| Patient Involvement | Rarely involved | Often notified and involved |
Why the Difference Matters
- Helps in faster, cleaner financial reconciliation.
- Reduces administrative burden on billing and accounts receivable teams.
- Ensures compliance with healthcare regulations.
- Protects provider reputation and strengthens patient trust.
Best Practices for Managing Reversals and Refunds
- Train Billing Teams: Clearly define reversal vs. refund steps.
- Verify Authorization: Prevent errors before claims submission.
- Audit Billing Processes: Catch issues early and stay compliant.
- Communicate with Patients: Keep transparency around financial transactions.