Quick Summary
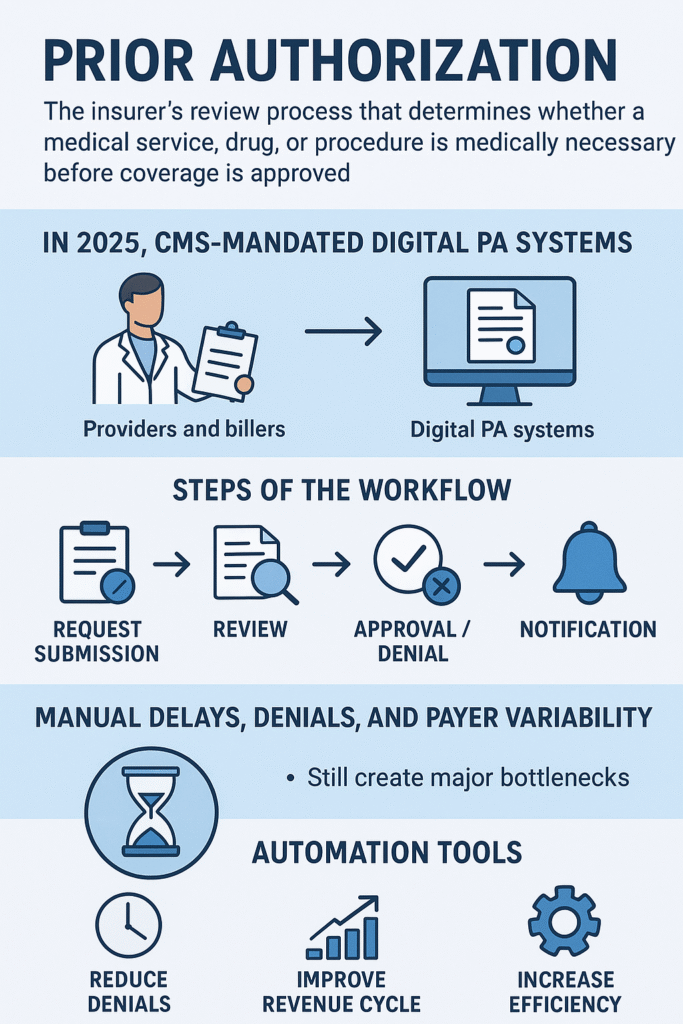
Prior authorization (PA) is the insurer’s review process that determines whether a medical service, drug, or procedure is medically necessary before coverage is approved. In 2025, CMS-mandated digital PA systems are transforming how providers and billers handle requests — but manual delays, denials, and payer variability still create major bottlenecks. Understanding each step of the workflow and the new automation tools can dramatically reduce denials and improve revenue cycle efficiency.
Also Read: How to Avoid Prior Authorization Delays in Healthcare in 2025
1. Understanding Prior Authorization
Prior authorization (often abbreviated as PA or pre-certification) is a utilization management process used by payers to decide whether a service or medication qualifies for reimbursement under a member’s policy.
In plain terms:
It’s the payer’s way of saying, “Show us why this is necessary before we pay for it.”
Providers must submit detailed clinical documentation to justify the request. The payer reviews it based on established coverage criteria, medical policies, and evidence-based guidelines (CMS, 2025).
If approved, services proceed without issue. If denied, the provider or patient must appeal — a process that can add days or weeks to care delivery.
2. Why Prior Authorization Exists
The main reason insurers use PA is cost control. According to the American Medical Association (AMA, 2024), over 90% of payers use prior authorization to prevent unnecessary or duplicative care.
Here’s what it’s designed to do:
- Ensure services are medically necessary
- Confirm that treatments follow plan coverage rules
- Encourage evidence-based care
- Avoid fraud or overutilization
While payers claim it improves efficiency, providers often experience the opposite. The AMA 2024 Prior Authorization Survey found:
- 88% of physicians reported delayed patient care
- 35% said PA led to adverse clinical outcomes
- 25% said PA resulted in treatment abandonment
These stats show that while PA reduces payer costs, it increases administrative burden across clinical and billing teams.
3. The Prior Authorization Workflow: Step-by-Step
Let’s walk through how PA actually works in a billing setting.
Step 1: Provider Identifies Service
A provider determines a test, procedure, or medication is needed.
Examples: MRI, CT scan, DME, biologic injection, or specialty drug.
Step 2: Check Payer Requirements
Each payer has its own PA requirement list. Billers must verify:
- CPT/HCPCS codes
- ICD-10 diagnosis codes
- Provider network status
- Place of service
This can be done via payer portals, EDI transactions, or payer API systems (CMS FHIR Implementation Guide, 2025).
Step 3: Submit Authorization Request
The billing or clinical team sends the request including:
- Patient demographics
- Provider NPI and tax ID
- CPT/ICD codes
- Supporting clinical notes
- Past treatment history
Requests are usually submitted through:
- Payer web portals (UnitedHealthcare, Aetna, Cigna)
- Clearinghouses (Availity, Change Healthcare)
- Integrated EHR/RCM platforms
Step 4: Payer Review
The payer’s utilization management (UM) department reviews:
- Medical necessity criteria
- Coverage guidelines
- FDA labeling (for drugs)
- CMS National Coverage Determinations (NCDs) or Local Coverage Determinations (LCDs)
If automated rules apply, AI-based screening may approve low-risk cases instantly.
Step 5: Payer Response
Three possible outcomes:
- Approved: Valid for a specific timeframe.
- Denied: Not medically necessary, not covered, or incorrect documentation.
- Pended: More documentation required.
Typical turnaround:
- Urgent: 24–72 hours
- Non-urgent: Up to 15 days
(CMS Prior Authorization Final Rule, 2025)
Also Read: The Prior Authorization Precision Protocol
4. Key Roles in the PA Process
- Ordering Provider: Determines clinical need.
- Billing/Authorization Specialist: Submits and tracks PA.
- Utilization Management Nurse/Reviewer: Reviews request for payer.
- Pharmacy Benefit Manager (PBM): Handles drug authorizations.
- Patient/Member: May need to sign forms or provide consent.
Each participant plays a role in reducing errors and delays. A weak link—usually incomplete documentation—triggers denials.
5. Common Services Requiring Prior Authorization
| Category | Common Examples |
|---|---|
| Imaging | MRI, CT, PET scans |
| Drugs | Biologics, specialty injectables |
| Surgeries | Elective orthopedic, bariatric, cosmetic |
| DME | CPAP, oxygen, wheelchairs |
| Rehab | Physical or occupational therapy |
| Home Health | Long-term or skilled nursing visits |
Even within these categories, requirements differ by payer and plan type (commercial, Medicare Advantage, Medicaid MCO).
6. Common Reasons for Denials
According to the CMS 2024 Denial Analytics Report, the top reasons include:
- Incomplete or missing documentation
- Incorrect CPT or ICD-10 coding
- Expired authorization period
- Out-of-network provider submission
- Service not medically necessary
- Late submission after service rendered
A denial can trigger:
- Claim rework (RFI)
- Appeal or peer-to-peer review
- Delayed reimbursement
For billers, this means lost productivity and cash flow disruption.
7. How Digital Prior Authorization Works in 2025
Here’s where things get interesting.
Starting January 1, 2026, CMS mandates major payers to implement electronic prior authorization (ePA) using FHIR APIs. Most commercial payers are already rolling it out in 2025.
What ePA Means
- Automation: Electronic data exchange replaces fax/email.
- Real-Time Status Updates: Providers see approval status instantly.
- Standardized Data: No more payer-specific forms.
- Faster Decisions: Payers must respond within 72 hours (urgent) or 7 days (non-urgent).
According to CMS (2025):
“The ePA system is designed to cut average response times from 14 days to under 72 hours, significantly reducing provider burden.”
Platforms like Epic Payer Platform, Availity Essentials, and Optum Intelligent Authorization already support real-time PA integration.
8. Workflow Integration for Clinics and Billers
Here’s how leading RCM teams now integrate PA into their workflow:
- Eligibility Check (270/271 Transaction): Confirm active coverage.
- PA Check: Use payer rules database or integrated API.
- Submit PA: Auto-populate forms with EHR data.
- Track Status: Real-time payer feedback via API.
- Store Authorization: Attach approval to patient record and claim.
- Claim Submission (837): Include authorization number in Loop 2300 REF segment.
This ensures compliance and prevents claim denials for “missing PA number.”
9. Case Example: Prior Authorization in Action
Case:
A cardiology practice submits a PA for CPT 93351 (stress echocardiogram).
- Payer: UnitedHealthcare
- Submission via Availity ePA Portal
- Documentation: Clinical notes + ICD-10 I20.0 (angina)
- Decision: Auto-approved by AI screening within 2 hours.
Result: No delay, no manual review.
Before automation, this same request took 2–3 business days.
That’s the kind of operational efficiency that’s redefining RCM performance benchmarks in 2025.
10. Tips to Avoid PA Delays and Denials
For Providers:
- Verify payer requirements before ordering tests or prescribing.
- Attach complete documentation (clinical notes, prior results).
- Use electronic PA tools integrated with EHR.
For Billers:
- Cross-check authorization number before claim submission.
- Maintain authorization logs by date and payer.
- Follow up daily on pending requests.
- Train staff on payer-specific submission portals.
For Both:
- Set internal PA turnaround KPIs (e.g., 90% within 3 days).
- Use dashboards or RPA bots to track requests automatically.
11. Financial and Operational Impact
Prior authorization is not just a compliance step; it’s a revenue cycle choke point.
According to MGMA (2024):
- Each manual PA costs $13.50–$18.50 in staff time.
- Average practice handles 45–60 PAs per week.
That’s thousands in hidden labor cost.
Automating even 50% of requests can improve:
- Cash flow by 20–30%
- Claim acceptance rates by 15%
- Patient satisfaction scores due to faster care initiation
12. Reform and Regulatory Outlook
Regulatory changes in 2025–2026 aim to streamline PA:
- CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F) mandates payer adoption of FHIR-based APIs for electronic requests.
- Payers must include PA decision details in standard EOBs.
- Providers can query coverage and PA status directly via EHR.
According to CMS Administrator Chiquita Brooks-LaSure (2025):
“This rule will save providers $15 billion annually by reducing administrative overhead and accelerating patient access to care.”
Several states — including Texas, Florida, and California — are also passing “gold card” laws, allowing providers with high approval rates to bypass PA for certain services.
13. The Human Element: Behind the Data
Technology aside, the real impact is personal.
Take Arthur, a 68-year-old patient with rheumatoid arthritis. His rheumatologist prescribed a biologic injection. The payer required PA, and it took three weeks to approve. By the time it cleared, his condition worsened, requiring hospitalization.
These delays ripple through patients’ lives and the provider’s revenue. That’s why billing teams must see PA not as paperwork — but as part of care delivery.
14. Future of Prior Authorization
By 2026, expect:
- Universal ePA adoption across commercial and government payers.
- Integration with AI-driven clinical decision tools.
- Reduction of low-risk, repetitive PAs.
- Predictive analytics for proactive submission.
The next step? “No-touch authorization” — where payer and provider systems auto-exchange data, and approvals happen in seconds for standardized services.
Key Takeaways
- Prior authorization is a mandatory pre-approval process required by payers to confirm medical necessity.
- In 2025, it’s shifting toward digital and AI-driven systems.
- Medical billers must align workflows with CMS ePA rules to reduce denials.
- Clinics that automate PA tracking gain significant financial and patient care advantages.
People Also Ask
It’s the process of obtaining payer approval before a service or procedure to ensure coverage.
With ePA, most approvals take 24–72 hours, compared to 10–14 days manually.
The claim will likely be denied, and the patient may be liable for the full cost.
By using EHR-integrated systems that connect to payer APIs for electronic PA submission and tracking.
No, but it’s evolving into a faster, more transparent, electronic system under CMS mandates.