In the ever-evolving world of medical billing, one system sits quietly behind the scenes, ensuring that providers are recognized, claims are processed, and compliance is maintained: PECOS. While it might not be as commonly discussed as coding practices or reimbursement strategies, PECOS (Provider Enrollment, Chain, and Ownership System) is an essential tool for medical billing professionals, particularly those working with Medicare.
This article explores PECOS in medical billing with comprehensive depth, from its foundational role to its practical use, troubleshooting, updates, and comparisons with other systems.
What Is PECOS in Medical Billing?
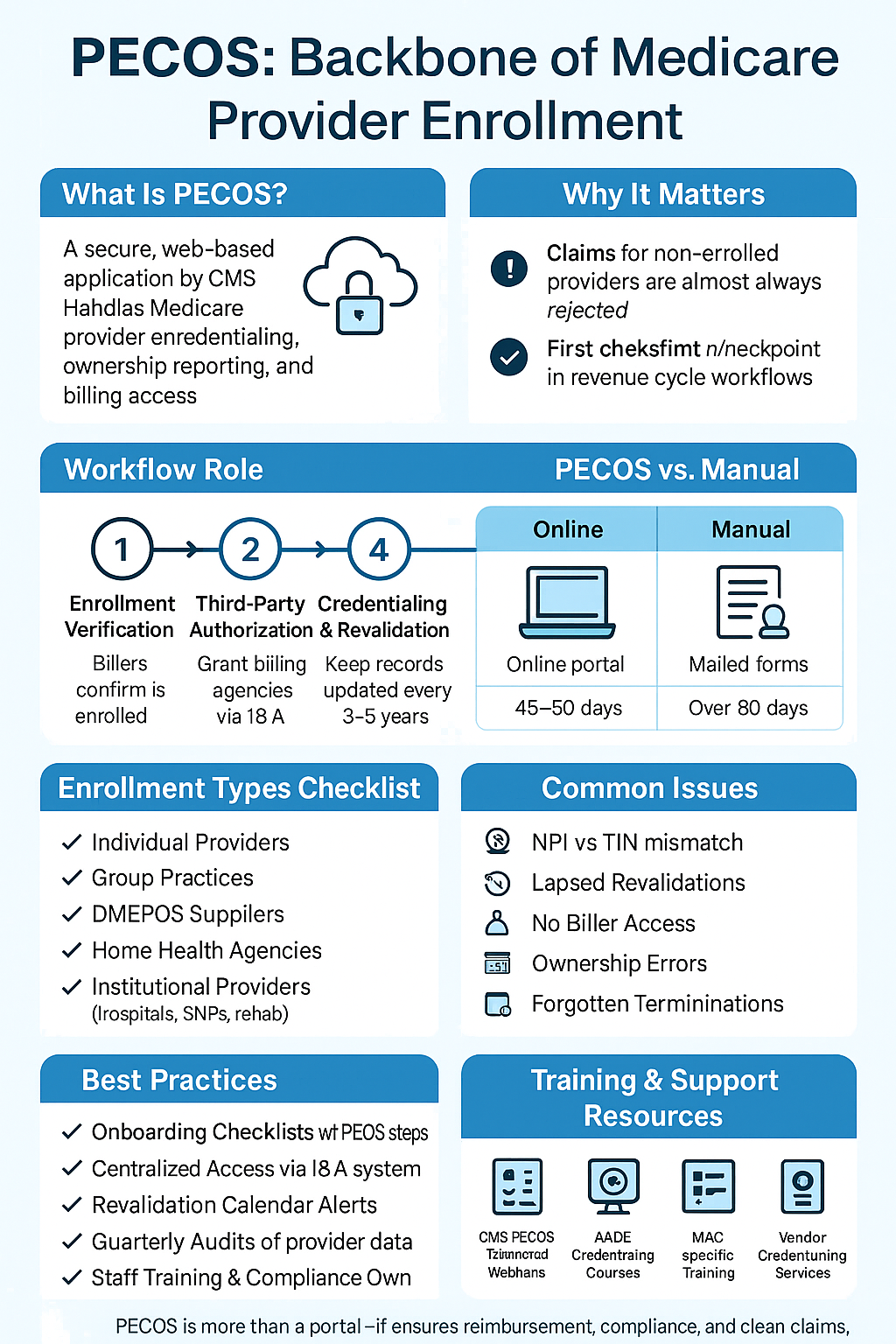
PECOS is a secure, web-based application developed and maintained by the Centers for Medicare & Medicaid Services (CMS). It serves as the official system for:
- Medicare provider enrollment
- Credentialing and revalidation
- Reporting chain ownership and affiliations
- Authorizing billing representatives and organizations
Introduced in response to increasing fraud concerns and administrative inefficiencies, PECOS replaced a cumbersome paper-based enrollment process with an automated digital solution. Today, it’s used by physicians, non-physician practitioners, DMEPOS suppliers, group practices, and hospitals to enroll in Medicare and maintain their active status.
In medical billing, PECOS is used to confirm whether a provider is actively enrolled and authorized to bill Medicare. If a provider isn’t in PECOS, any claims submitted on their behalf are likely to be rejected—regardless of how accurately they’re coded or documented.
The Role of PECOS in Medical Billing Workflows
PECOS acts as the first checkpoint in the revenue cycle when dealing with Medicare patients. Here’s how it fits into daily billing operations:
- Enrollment Verification: Billers use PECOS to check a provider’s Medicare participation and billing eligibility.
- Third-Party Authorization: PECOS enables billing companies to act on behalf of providers by being granted access through the Identity & Access (I&A) system.
- Credentialing & Revalidation: Providers must routinely update their information and revalidate their enrollment every 3-5 years.
- Change Management: PECOS allows users to report changes to addresses, group affiliations, ownership, and licensure.
Failure to use PECOS properly can result in:
- Claim denials
- Payment delays
- Compliance violations
- Potential penalties or exclusion from the Medicare program
How to Access PECOS: A Step-by-Step Guide
Step 1: Set Up an Identity & Access Management (I&A) Account
Every provider must first create a profile through the CMS I&A System, which links their NPI and credentials to PECOS. Billing agencies or credentialing staff must also register if they are authorized users.
Step 2: Log In to PECOS
Visit https://pecos.cms.hhs.gov/pecos/ and use the login credentials associated with the provider or authorized official.
Step 3: Choose Your Enrollment Type
Options include:
- Individual practitioner
- Group practice
- DMEPOS supplier
- Organizational provider
Step 4: Complete Application
This involves filling out:
- Personal and business information
- Practice locations
- Ownership details
- Licensure and certifications
- EFT banking info
Step 5: Sign and Submit
Once completed, the application is submitted electronically, and CMS initiates the verification process. Providers or their representatives can track the application status through PECOS or via email.
PECOS Enrollment Types and Who Should Use Them
Depending on the type of entity, PECOS enrollment pathways may differ:
| Provider Type | PECOS Enrollment Needed? | Notes |
|---|---|---|
| Physicians & NPPs | Yes | Individual enrollment with option to link to group |
| Group Practices | Yes | Organization must enroll and link practitioners |
| DMEPOS Suppliers | Yes | Subject to additional accreditation and inspection |
| Home Health Agencies | Yes | Often require revalidation every 3 years |
| Institutional Providers | Yes | Includes hospitals, SNFs, rehab centers |
| Telehealth Providers | Yes | Must meet Medicare’s distant site requirements |
PECOS vs Manual Enrollment: A Modern Comparison
Before PECOS, providers had to complete a paper CMS-855 form and mail it to a MAC (Medicare Administrative Contractor). PECOS eliminated this tedious process.
| Feature | PECOS | Manual Enrollment |
| Submission Method | Online via CMS portal | Paper-based forms |
| Time to Process | 45-60 days | 90+ days |
| Document Storage | Centralized and electronic | Physical copies |
| Signature Collection | Digital or scanned | Wet ink required |
| Status Tracking | Real-time | Manual follow-up with MAC |
How to Verify PECOS Enrollment
You can verify whether a provider is actively enrolled through:
- The PECOS NPI Search Tool
- MAC (Medicare Administrative Contractor) portals
- CMS Medicare Enrollment Lookup Tool
Verification is especially critical when:
- Hiring a new provider
- Adding a locum tenens or substitute provider
- Submitting claims on behalf of a contractor
Failure to verify can result in Medicare denials or payment holds.
Common Issues in PECOS for Medical Billing
1. Mismatched NPIs and TINs
When the provider’s Tax Identification Number doesn’t match their National Provider Identifier, claims are flagged.
2. Revalidation Delays
CMS requires providers to revalidate every 3-5 years. Missing this window can cause deactivation.
3. Lack of Access for Billers
Billing teams often lack delegated access and are unable to update information or check application status.
4. Errors in Ownership Details
Especially in group practices, unclear ownership structures can cause CMS to reject or delay approval.
5. Forgotten Terminations
Providers who retire or leave a group must be properly terminated in PECOS. If not, claims can route incorrectly.
Best Practices for PECOS Management in Medical Billing
- Create Onboarding Checklists: Include PECOS verification as a standard step.
- Centralize Access: Use the I&A system to ensure all billers and credentialers have appropriate permissions.
- Track Revalidation Cycles: Use a calendar-based system to track when providers are due for revalidation.
- Conduct Regular Audits: Quarterly checks can catch outdated licensure or bank details.
- Educate Staff: Provide PECOS training for new billing hires or assign a compliance lead to monitor activity.
PECOS Alternatives for Non-Medicare Billing
While PECOS is the gold standard for Medicare, private and Medicaid payers often use:
- CAQH ProView for commercial payer credentialing
- State Medicaid Portals
- Payer-Specific Portals (e.g., UHC, Cigna)
Understanding how PECOS fits into a broader credentialing strategy is vital for full revenue cycle integrity.
Training & Support Resources for PECOS
To build proficiency:
- CMS PECOS Tutorials & Webinars: Found on the official CMS website
- AAPC Courses: Offer credentialing and Medicare-focused modules
- MAC-Specific Webinars: Medicare contractors often host live and recorded PECOS training
- Vendor Credentialing Services: Outsourced options for busy practices or hospitals
Conclusion: PECOS Is More Than Just a Portal
PECOS in medical billing is not merely a software system—it’s the foundation of Medicare enrollment and claim eligibility. Its integration into every part of the provider lifecycle—from onboarding to updates and revalidations—makes it indispensable.
For medical billers, understanding how to navigate PECOS can prevent thousands in lost reimbursements, reduce denials, and streamline compliance. With proper training, checklists, and access management, PECOS becomes a powerful ally in ensuring clean claims and optimized revenue.