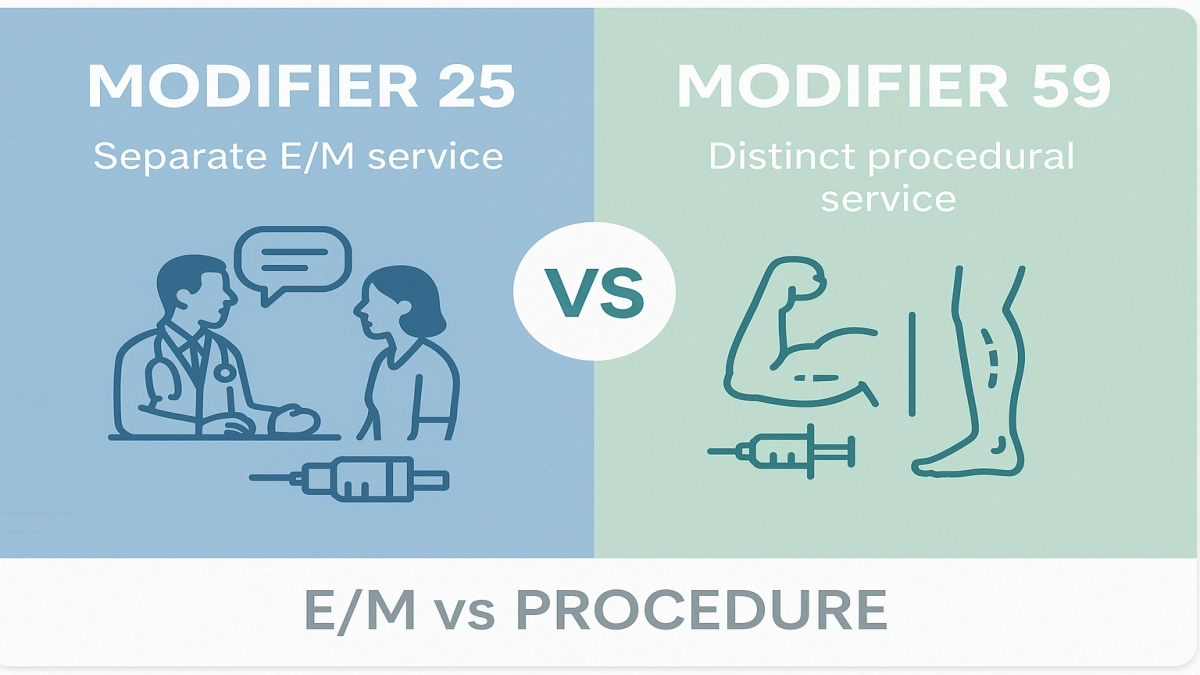
In the world of medical billing, the tiniest details can make the biggest difference—especially when it comes to modifiers. Two of the most commonly misunderstood are modifier 25 and modifier 59. To the untrained eye, they may seem interchangeable. But in reality, using the wrong one could trigger denials, audits, or even compliance issues.
If you’re a medical coder, billing specialist, or physician, understanding the difference between modifier 25 vs 59 is essential—not just for getting claims paid, but for staying on the right side of payer policies.
This guide will walk you through the critical distinctions, proper usage, and best practices for each, all while keeping it real and relatable.
What Is Modifier 25 in Medical Billing?
Modifier 25 indicates that a significant, separately identifiable evaluation and management (E/M) service was performed by the same physician on the same day as another procedure.
✅ When to Use Modifier 25:
- The patient comes in for a scheduled procedure, but also presents a new or significantly worsened complaint.
- The E/M service goes beyond the typical pre- and post-op care of the procedure.
- Proper documentation exists to support that both services were necessary and distinct.
🔍 Example: A patient comes in for a skin lesion removal but also reports chest pain. The provider performs a full cardiac exam. Modifier 25 is appended to the E/M code to show it was not bundled with the lesion removal.
What Is Modifier 59 in Medical Billing?
Modifier 59 is used to identify procedures or services that are not normally reported together, but are appropriate under the circumstances because they were performed in a different session, site, or organ system.
✅ When to Use Modifier 59:
- You’re billing two procedures that typically bundle, but in this case, they were performed independently.
- The services occurred in different anatomic sites, different encounters, or separate incisions.
- No other more appropriate modifier applies (e.g., XS, XP, XE, XU).
🔍 Example: A provider performs physical therapy on the right shoulder and manual therapy on the left hip—two services typically bundled. Modifier 59 justifies that these were distinct procedures.
💡 Key Difference Between Modifier 25 vs 59
| Modifier | Used For | Applies To | Indicates | Often Used With |
|---|---|---|---|---|
| 25 | E/M services | Same physician, same day | A significant, separate E/M service | Minor procedures |
| 59 | Procedural services | Same or different provider | A distinct procedural service | Surgical or diagnostic CPTs |
⚖️ How to Choose Between Modifier 25 and 59
Modifier 25:
- Use only with E/M codes.
- Ensure documentation shows a distinct, medically necessary evaluation.
- Best for office visits + minor procedures on the same day.
Modifier 59:
- Use with CPT codes for procedures, not E/M.
- Must prove the services were not integral to one another.
- Best for bundled procedure code pairs with a valid reason for separation.
🧠 Common Mistakes to Avoid
❌ Using Modifier 25 on a procedure code
Modifier 25 should never be used with surgical or procedural CPTs. It’s exclusive to E/M codes.
❌ Using Modifier 59 when another X-modifier is more specific
If CMS X-submodifiers apply (XS, XP, XE, XU), they should be used instead of 59.
❌ Lack of documentation
Both modifiers require clear documentation that justifies why services are separate and payable.
🎯 Best Practices for Modifier 25
- Only apply when the E/M service is above and beyond the norm.
- Keep time-stamped progress notes to support both services.
- Use modifier 25 sparingly; overuse can trigger audits.
🎯 Best Practices for Modifier 59
- Only use when procedures are truly distinct.
- Know the Correct Coding Initiative (CCI) edits—this tells you when procedures are normally bundled.
- When applicable, consider using X{E/U/S/P} modifiers for more specificity.
🔄 Real-World Scenarios: Modifier 25 vs 59 in Action
Scenario 1: Same Day Visit + Procedure
A patient arrives for a wart removal (CPT 17110) but also discusses worsening asthma symptoms.
Correct use: Add modifier 25 to the E/M code (e.g., 99213-25).
Scenario 2: Distinct Procedures, Same Day
A chiropractor performs manual therapy (97140) and therapeutic exercise (97110) on different body parts.
Correct use: Add modifier 59 to the second CPT code (97140-59).
🧭 Modifier 25 vs 59 for Physicians, Billers, and Coders
- Physicians should understand the clinical criteria that justify separate billing.
- Billers need to verify that documentation and coding align for payer compliance.
- Coders must check CCI edits and apply modifiers appropriately to avoid denials or audits.
📝 Documentation Tips: What Payers Look For
- Modifier 25: Look for separate SOAP notes or a clearly defined, separate reason for the E/M service.
- Modifier 59: Include documentation of anatomical site differences, timing, or distinct session.
✅ Quick Checklist: When to Apply Each Modifier
🗂️ Modifier 25
- Was an E/M code billed?
- Was there a separate, identifiable service beyond pre/post-op?
- Does documentation support the distinction?
🗂️ Modifier 59
- Are the CPT codes bundled under NCCI edits?
- Were the procedures performed in a different site/session/approach?
- Can another modifier (like XS or XE) be used instead?
🔗 Internal Linking Suggestions
If your blog covers these topics, link internally to:
- “How to Read NCCI Edits Like a Pro”
- “Top Denial Reasons for Modifier Errors—and How to Fix Them”
- “X Modifiers Explained: The Modern Alternative to Modifier 59”
🎁 Takeaways: Use With Care, Bill With Confidence
- Modifier 25 is for significant E/M services on the same day as procedures.
- Modifier 59 is for separating procedures that are normally bundled.
- Both require excellent documentation, clinical justification, and judicious use.
When used correctly, these modifiers help ensure providers are fairly reimbursed, while maintaining compliance and avoiding denials.