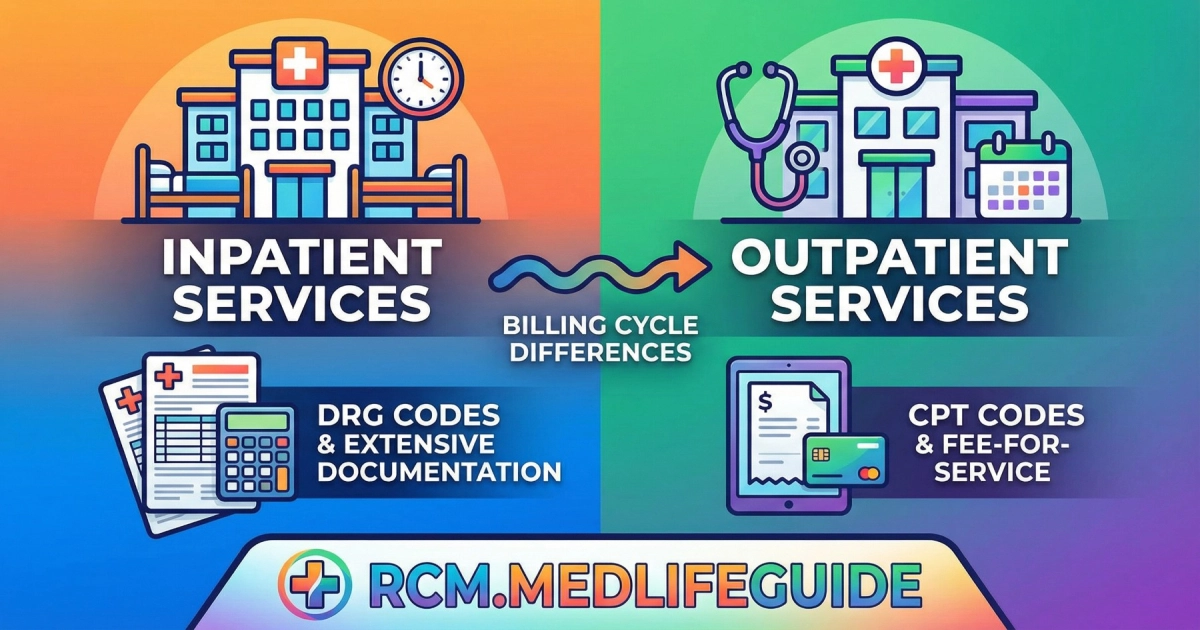
Inpatient and outpatient billing differ based on admission status, scope of care, coding systems, and payment methods. Inpatient billing applies to hospital stays that usually cross two midnights, using DRG-based bundled payments. Outpatient billing covers short-term or same-day services, using CPT/HCPCS codes and itemized or APC-based payments. Accurate understanding is crucial for revenue, compliance, and avoiding billing errors.
What Is Inpatient Billing?
Imagine a patient admitted for a severe pneumonia infection. They stay in the hospital under a physician’s order for continuous care. This is inpatient billing in action.
Key Points:
- Scope: Covers the entire hospital stay, including room, nursing, surgeries, medications, labs, and supplies.
- Unit of Service: Days of stay; the entire episode of care is billed.
- Payment Method: Bundled via Diagnosis-Related Groups (DRGs).
- Documentation: Requires admission orders, daily progress notes, procedure reports, and discharge summaries.
Hook: Hospitals must carefully document every aspect of an inpatient stay, because even a single missing note can trigger audit scrutiny.
What Is Outpatient Billing?
Consider a patient visiting for a same-day knee arthroscopy. They arrive in the morning, have the procedure, and leave by evening. This is outpatient billing.
Key Points:
- Scope: Individual, itemized services such as labs, imaging, minor procedures, or emergency visits.
- Unit of Service: Each service or procedure is billed separately.
- Payment Method: Fee-for-Service (FFS) or Ambulatory Payment Classification (APC) system.
- Documentation: Focuses on each service, using CPT/HCPCS codes.
Hook: Even a short outpatient visit can involve dozens of line items on a claim form, each needing precise coding.
Core Differences: Inpatient vs Outpatient Billing
| Feature | Inpatient (IP) | Outpatient (OP) |
|---|---|---|
| Admission Trigger | Formal physician order, expected stay of two midnights or more | Services completed in less than 24 hours or observation status |
| Scope of Billing | Entire hospital stay (room, board, medications, procedures) | Specific services, procedures, and supplies |
| Unit of Service | Days of stay; episode of care | Individual services or units (e.g., labs, procedures, therapy) |
| Payment Model | Bundled payment under DRG / PPS | Itemized payment under Fee-for-Service or APC |
| Coding – Diagnosis | ICD-10-CM | ICD-10-CM |
| Coding – Procedure | ICD-10-PCS | CPT / HCPCS Level II |
| Primary Billing Form | UB-04 (institutional claim) | UB-04 (institutional claim), itemized differently |
| Documentation Complexity | High – requires full admission, progress notes, discharge summary | Moderate – focused on specific service documentation |
Hook: Understanding this table can save billing teams from costly mistakes and rejected claims.
1. Admission Status
Inpatient: Patients expected to stay two midnights or more are formally admitted. Billing covers the full episode of care, including ancillary services.
Outpatient: Patients receive treatment but are not admitted. Services are billed individually. Observation stays are technically outpatient even if they stay overnight.
Micro-story: A patient treated for chest pain may spend 36 hours under observation. The hospital codes it as outpatient, not inpatient, despite the overnight stay. A misclassification could trigger audits and delays in payment.
2. Coding Systems
Inpatient:
- Diagnosis: ICD-10-CM
- Procedure: ICD-10-PCS
- Purpose: Codes feed into DRG assignment, determining the bundled payment.
Outpatient:
- Diagnosis: ICD-10-CM
- Procedure: CPT / HCPCS Level II
- Purpose: Codes feed into APC payment or FFS reimbursement, covering each service individually.
Hook: One wrong CPT code can reduce reimbursement significantly—precision matters.
3. Payment Methods
Inpatient: Uses Prospective Payment System (PPS). The hospital receives one bundled payment for the entire stay. If costs exceed the DRG rate, the hospital absorbs the loss; if costs are lower, they keep the savings.
Outpatient: Uses Fee-for-Service (FFS) or APC. Each service has a set payment. Missed services or miscodes directly reduce revenue.
Micro-story: A hospital coded a minor outpatient lab incorrectly. The claim underpaid by $250. That single mistake highlights why outpatient billing demands attention to detail.
4. Documentation Requirements
Inpatient: Comprehensive — includes admission orders, progress notes, surgeries, medications, and discharge summaries.
Outpatient: Focused — each service documented separately, with CPT/HCPCS codes, modifiers, and units.
Hook: Proper documentation is the backbone of compliance. Even small omissions can result in audits, penalties, or delayed payments.
5. Observation Status
- Observation stays are technically outpatient, even if they last overnight.
- Hospitals monitor patients closely but do not meet inpatient criteria unless the two-midnight expectation is documented.
Micro-story: Observation patients often confuse billing statements, seeing “hospital charges” without realizing the services are itemized under outpatient billing rules.
Why Understanding These Differences Matters
- Revenue Accuracy: Correct classification ensures proper reimbursement.
- Compliance: Avoids audits from CMS, RAC, OIG, and commercial payers.
- Operational Efficiency: Helps providers, coders, and billing staff coordinate effectively.
- Patient Communication: Reduces confusion over charges and co-pays.
Hook: Even experienced billing staff review the inpatient vs outpatient status daily—accuracy is critical.
People Also Ask
- What makes a patient inpatient vs outpatient?
Doctors determine inpatient status based on the two-midnight rule. Shorter stays are outpatient. - Why do inpatient stays use DRGs?
DRGs bundle all hospital services for the stay into a single payment, simplifying reimbursement and controlling costs. - Why does outpatient billing use CPT codes?
CPT codes describe each specific service rendered, which is essential for itemized billing. - What is observation status?
Observation is an outpatient classification for patients monitored overnight or longer without formal admission. - Can billing mistakes trigger audits?
Yes. Misclassifying stays or using incorrect codes can lead to CMS, RAC, OIG, or commercial payer audits.
Conclusion
The difference between inpatient and outpatient billing is crucial for accurate hospital reimbursement and compliance. Inpatient billing bundles services under DRGs for longer stays, while outpatient billing is itemized per service using CPT/HCPCS codes. Proper coding, documentation, and classification protect revenue, prevent audits, and improve patient understanding of bills.
Author Bio:
This article was written and reviewed by a medical billing and coding specialist with extensive experience in inpatient and outpatient hospital billing. It simplifies complex billing rules for healthcare professionals and beginners alike.
Disclaimer:
This content is for informational purposes only and is not a substitute for professional medical or billing advice. Always consult qualified experts for guidance.
People Also Ask
The main factor is whether the doctor expects the patient to need hospital care crossing two midnights. This rule is defined by CMS.
DRGs allow Medicare to pay a single bundled amount for the whole stay. It helps control costs and standardize payments.
CPT codes describe the exact service performed. Outpatient care is itemized, so each service needs its own code.
Observation is outpatient monitoring. Even if a patient stays overnight, they might still be outpatient if they do not meet the Two-Midnight Rule.
Yes. Incorrect inpatient or outpatient classification can trigger MAC, RAC, OIG, or commercial payer audits.