Whether you’re handling billing in a nephrology clinic or navigating the world of chronic kidney disease (CKD) as a patient or provider, one thing remains clear—ICD 10 codes for kidney care are essential for everything from proper reimbursement to effective care coordination.
In this guide, we’ll decode the complexity behind ICD 10 for kidney care, break down the most relevant codes, address common billing pitfalls, and give you the tools to ensure accuracy, compliance, and better patient outcomes.
What Is ICD 10 and How Does It Relate to Kidney Care?
The International Classification of Diseases, 10th Revision (ICD-10), is a standardized system used to code diagnoses and health conditions. In kidney care, ICD-10 codes help document conditions like:
- Chronic Kidney Disease (CKD)
- Acute Kidney Injury (AKI)
- Glomerulonephritis
- Dialysis-related complications
- Hypertensive nephropathy
Without the correct code, a claim could be denied, or worse, a patient’s care plan could lack important clinical clarity.
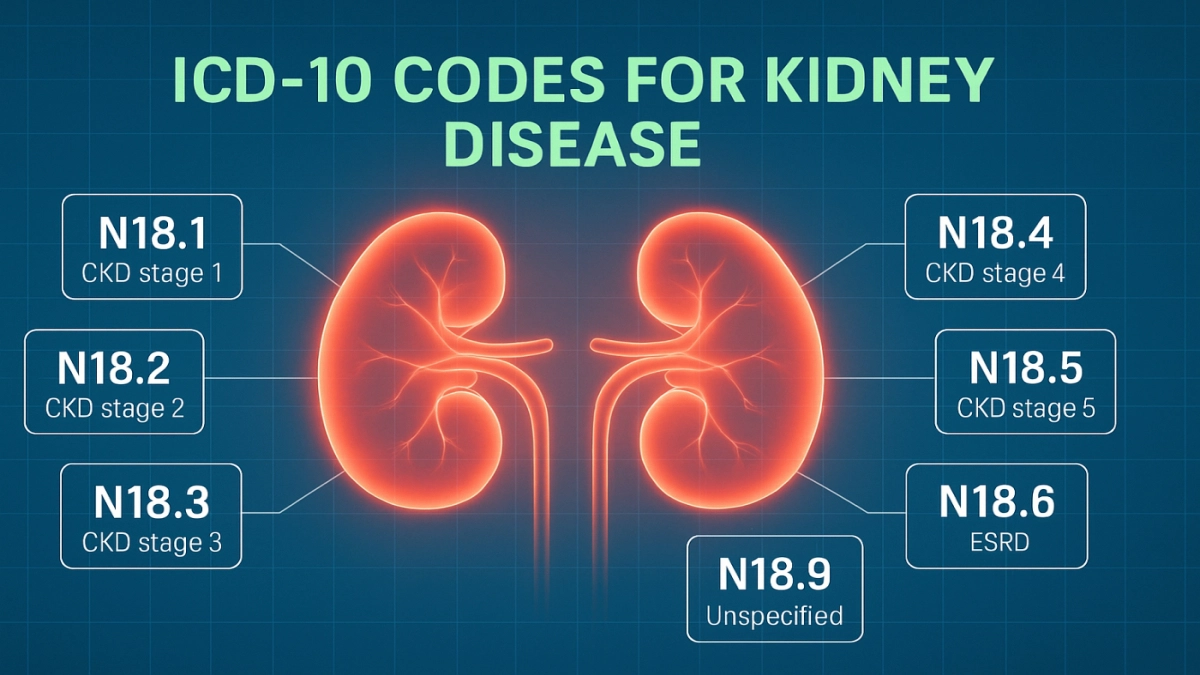
Top ICD 10 Codes for Kidney Care
Here’s a breakdown of the best ICD 10 codes for kidney disease documentation, based on condition category:
Chronic Kidney Disease (CKD):
| ICD 10 Code | Description |
|---|---|
| N18.1 | CKD Stage 1 |
| N18.2 | CKD Stage 2 (Mild) |
| N18.3 | CKD Stage 3 (Moderate) |
| N18.4 | CKD Stage 4 (Severe) |
| N18.5 | CKD Stage 5 |
| N18.6 | End-Stage Renal Disease (ESRD) |
These are often paired with comorbidities such as diabetes (E11.22 – Type 2 with CKD) or hypertension (I12.0 – Hypertensive CKD with Stage 1-4).
Acute Kidney Injury (AKI):
| ICD 10 Code | Description |
|---|---|
| N17.0 | AKI with tubular necrosis |
| N17.1 | AKI with acute cortical necrosis |
| N17.9 | AKI, unspecified |
ICD 10 vs ICD 9 for Kidney Care: What’s Changed?
Before ICD-10, kidney disease was often coded using vague or overly broad categories in ICD-9 (like 585.x for CKD). The shift to ICD-10 allows for:
- Greater specificity (e.g., CKD stage differentiation)
- Improved data analysis
- Enhanced billing precision
- Better coordination across providers and payers
This upgrade isn’t just administrative—it’s clinically impactful.
How to Choose the Right ICD 10 Code for Kidney Care
Here’s a quick step-by-step for medical billers and providers:
- Identify the Kidney Condition Type
(CKD? AKI? Glomerulonephritis? Cystic disease?) - Determine Specific Stage or Etiology
Staging is vital for CKD. Check lab data (e.g., eGFR) and clinical documentation. - Include Comorbid Conditions
Common comorbidities include:- Diabetes (E11.22)
- Hypertension (I12.9 or I13.0)
- Heart failure (I50.9)
- Use Multiple Codes if Needed
A patient with CKD Stage 3 and uncontrolled Type 2 diabetes may need both N18.3 and E11.65. - Review for Modifier Requirements
Especially when procedures like dialysis (Z99.2) or transplant status (Z94.0) are involved.
ICD 10 Coding for Dialysis and Kidney Transplants
| ICD 10 Code | Use Case |
|---|---|
| Z99.2 | Dependence on renal dialysis |
| Z91.15 | Noncompliance with dialysis |
| Z94.0 | Kidney transplant status |
| T86.10 | Kidney transplant complication, unspecified |
These are vital for tracking complications, continuity of care, and justifying services like ESRD management, access placement, or transplant evaluations.
Common ICD 10 Coding Errors in Kidney Care (and How to Avoid Them)
- Coding CKD without a stage
→ Always use the appropriate N18.x code for staging. - Omitting comorbidities
→ Missing a diabetes or hypertension code leads to under-documentation. - Using outdated or unspecified codes
→ Avoid N18.9 (CKD unspecified) unless there’s no clinical data. - Failing to update codes after progression
→ CKD patients often progress—ensure codes reflect current stage, not historical.
Best Practices for ICD 10 Kidney Coding
- Use most specific code available
Vague coding (e.g., N18.9) can delay claims and create documentation gaps. - Review labs and provider notes before coding
Match codes to recent eGFR values and clinical status. - Educate providers on documentation gaps
Especially in outpatient nephrology or dialysis centers. - Update codes when disease progresses
CKD Stage 3 can become Stage 4—coding should reflect that. - Audit high-volume codes quarterly
Spot patterns, inconsistencies, or overuse of unspecified codes.
ICD 10 Resources for Kidney Care Professionals
Looking to level up your skills? Here are trusted training resources:
- CMS ICD-10 Guidelines for Nephrology
- AHIMA kidney-specific coding webinars
- KDIGO (Kidney Disease: Improving Global Outcomes) staging charts
- American Kidney Fund (AKF) for documentation tips
Consider adding a personal note or review if you’ve used any of these.
Benefits of Using ICD 10 in Kidney Disease Management
- Better care planning based on disease stage
- Accurate reimbursement for complex renal services
- Early detection tracking with screening codes (Z13.6)
- Enhanced coordination with primary care, endocrinology, and cardiology
Actionable Takeaways
- Always include staging when coding for CKD.
- Pair kidney-related ICD-10 codes with diabetes, hypertension, and dialysis status when applicable.
- Review latest ICD-10 updates each October to ensure compliance.
- Avoid N18.9 unless truly necessary—it signals missing documentation.
- Train staff on kidney-specific audit risks in billing.