Upcoding and downcoding are billing practices in medical coding—but they have very different implications.
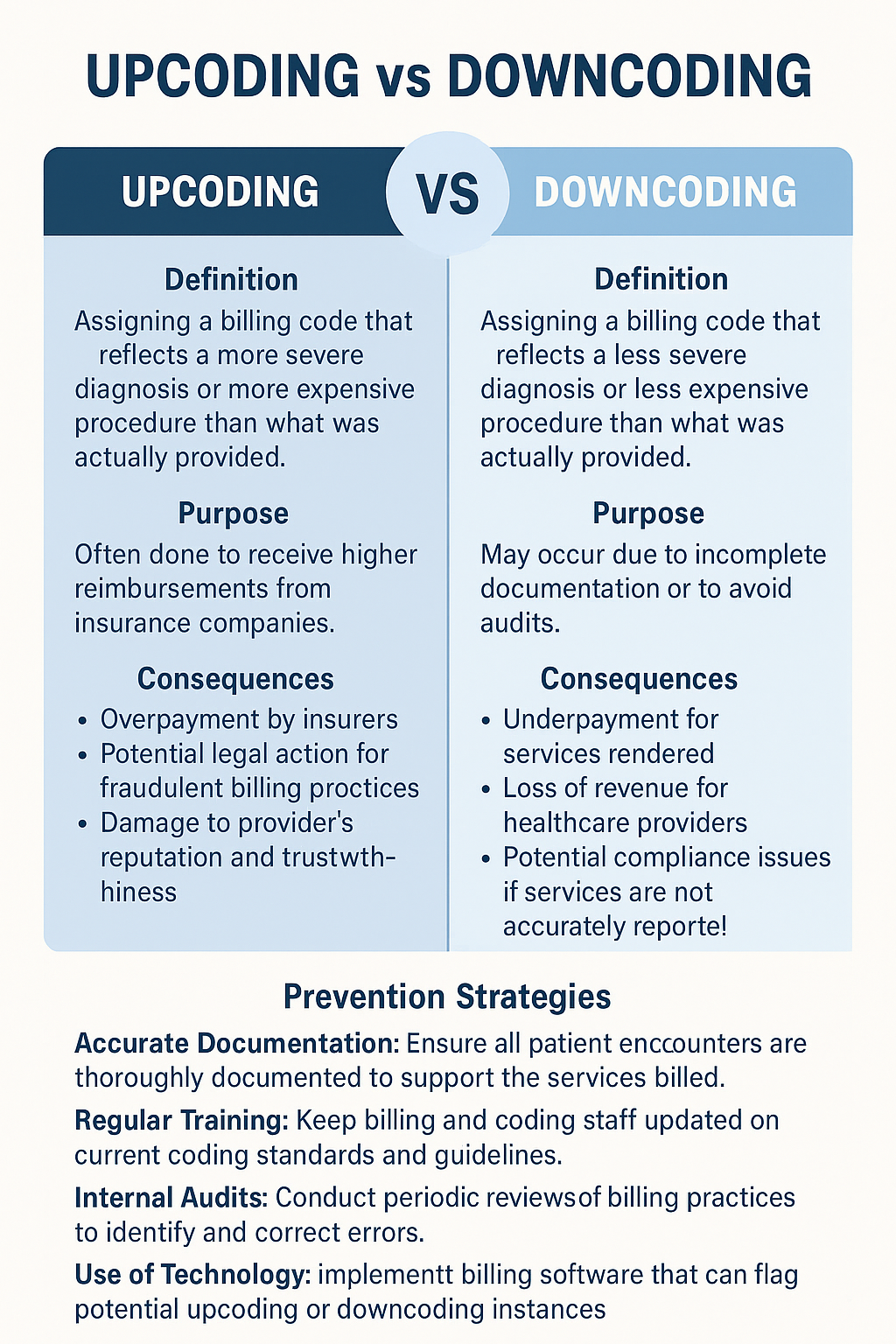
Upcoding is when a healthcare provider uses billing codes for more severe diagnoses or procedures than what was actually performed, often to receive higher reimbursement. Downcoding, on the other hand, is when the billing code reflects a less severe or lower-cost service than what was provided, sometimes done out of caution or by mistake.
Why Are Upcoding and Downcoding Important?
Understanding these terms helps protect both patients and providers. Upcoding can lead to overcharging, while downcoding can result in lost revenue or underreporting of care.
From a legal standpoint, both practices can raise compliance issues. Insurance companies and government programs like Medicare may investigate claims suspected of being inaccurately coded.
Are Upcoding and Downcoding Illegal?
Yes, both practices can be considered illegal if done fraudulently.
Intentional upcoding is a form of healthcare fraud and can lead to audits, penalties, or even criminal charges. Downcoding, though less frequently prosecuted, can also violate billing compliance rules if it misrepresents services provided.
📊 Chart: Risk Comparison of Coding Practices
| Coding Practice | Revenue Impact | Legal Risk | Common Intent |
|---|---|---|---|
| Accurate Coding | Fair & Balanced | Low | Ethical Billing |
| Upcoding | Increases Revenue | High (Fraud Risk) | Inflate Reimbursement |
| Downcoding | Decreases Revenue | Moderate | Avoid Audit / Errors |
How to Prevent Upcoding and Downcoding
To avoid these risks, providers should implement strong internal auditing and staff training programs.
Using AI-assisted coding tools can also reduce human error, and regular chart reviews help ensure that the services rendered match the codes submitted.
Final Thoughts: Ethical Coding Matters
Whether you’re a patient, provider, or billing specialist, knowing the difference between upcoding and downcoding helps maintain trust and transparency in healthcare.
Medical coding should reflect the true nature of care—nothing more, nothing less. Staying informed helps everyone make smarter, more ethical decisions.
Frequently Asked Questions
Upcoding is billing for a higher-level service than provided, often to increase reimbursement. It may occur due to fraud, errors, or aggressive billing.
Downcoding is using a lower-level code than justified, reducing reimbursement. It may occur due to incomplete documentation, audit fears, or payer adjustments.
Upcoding: Assigning a higher-paying CPT/ICD code than supported by documentation.
Downcoding: Using a lower-paying code than warranted, often due to insufficient documentation.
A provider documents a Level 4 office visit (complex care) but the coder assigns a Level 3 code because the note lacks detailed medical decision-making.
Overcoding: Billing for unnecessary or excessive services (e.g., extra tests not medically needed).
Upcoding: Billing a higher-level code for a single service (e.g., coding a moderate procedure as complex). Both can be fraudulent, but overcoding involves quantity, while upcoding involves severity.