Bundling in CPT coding means combining multiple services into one code for billing, while unbundling is separating them out to bill each individually.
Bundling is often required to follow payer rules and avoid overbilling, while unbundling (when appropriate) ensures every provided service gets recognized. Correct usage protects against claim denials, audits, and compliance risks.
What Is Bundling in CPT Coding?
Bundling occurs when related procedures are grouped under one CPT code instead of billing separately for each step. This happens because insurance companies expect that certain services are naturally part of a bigger procedure and shouldn’t be charged individually.
For example, suturing a wound after surgery is considered bundled—it’s expected and already included in the surgical code.
| Example of Bundling | Description |
|---|---|
| Surgical procedure + wound closure | Closure is bundled into the main surgical code |
✅ Tip: Check NCCI edits (National Correct Coding Initiative) for bundled code rules before billing!
What Is Unbundling in CPT Coding?
Unbundling means billing separately for procedures that are normally combined. Sometimes unbundling is necessary—like when a patient truly receives independent services that aren’t part of the main procedure.
However, unbundling incorrectly (to increase reimbursement) is considered fraud and can trigger audits or fines.
| Correct Unbundling Example | When it’s justified |
|---|---|
| Two unrelated surgeries during the same session | Different anatomical sites, separate problems |
✅ Tip: Use modifiers like Modifier 59 to explain why services are separately reportable.
Why Bundling and Unbundling Matters
Bundling and unbundling directly impact reimbursement, compliance, and patient billing clarity.
Getting it wrong can cause:
- Denied claims
- Underpayment or overpayment
- Legal action for improper billing
Correct coding based on clear CPT guidelines and payer rules maintains ethical standards and financial health for providers.
Common Modifiers Used in Bundling and Unbundling
Using CPT modifiers correctly clarifies billing intent. Some important ones include:
| Modifier | Meaning |
|---|---|
| Modifier 59 | Distinct procedural service |
| Modifier 25 | Significant, separately identifiable E/M service |
| Modifier 51 | Multiple procedures during the same session |
✅ Tip: Always document clearly why you used a modifier to avoid denials.
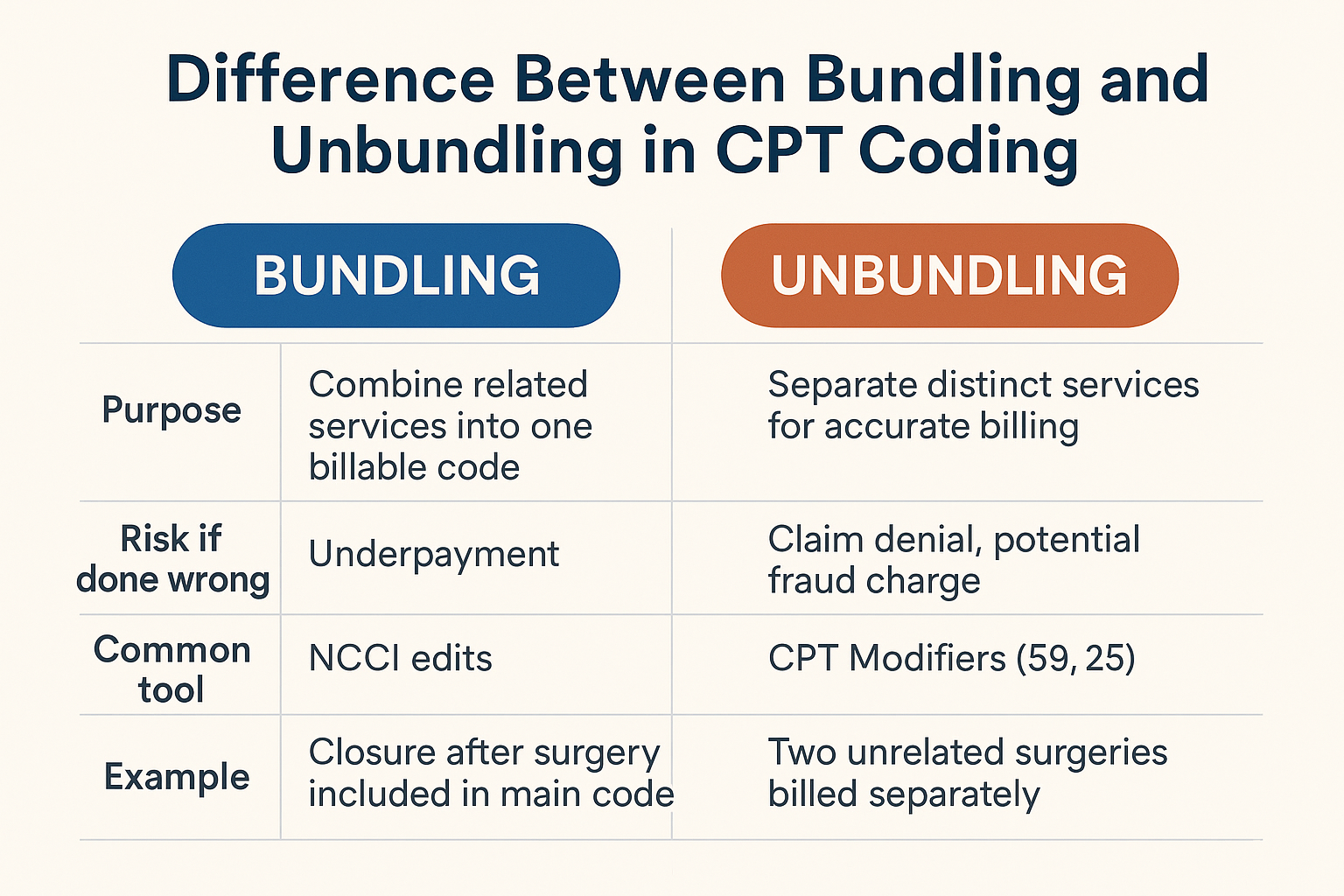
Bundling vs. Unbundling at a Glance
Here’s a simple visual breakdown:
| Aspect | Bundling | Unbundling |
|---|---|---|
| Purpose | Combine related services into one billable code | Separate distinct services for accurate billing |
| Risk if done wrong | Underpayment | Claim denial, potential fraud charge |
| Common tool | NCCI edits | CPT Modifiers (59, 25) |
| Example | Closure after surgery included in main code | Two unrelated surgeries billed separately |
Final Thoughts: Coding with Accuracy and Integrity
Mastering bundling and unbundling isn’t just about getting paid—it’s about billing ethically, staying compliant, and protecting patients and practices.
Follow payer policies, document thoroughly, use the right modifiers, and when unsure, always review NCCI edits or ask a certified coder.