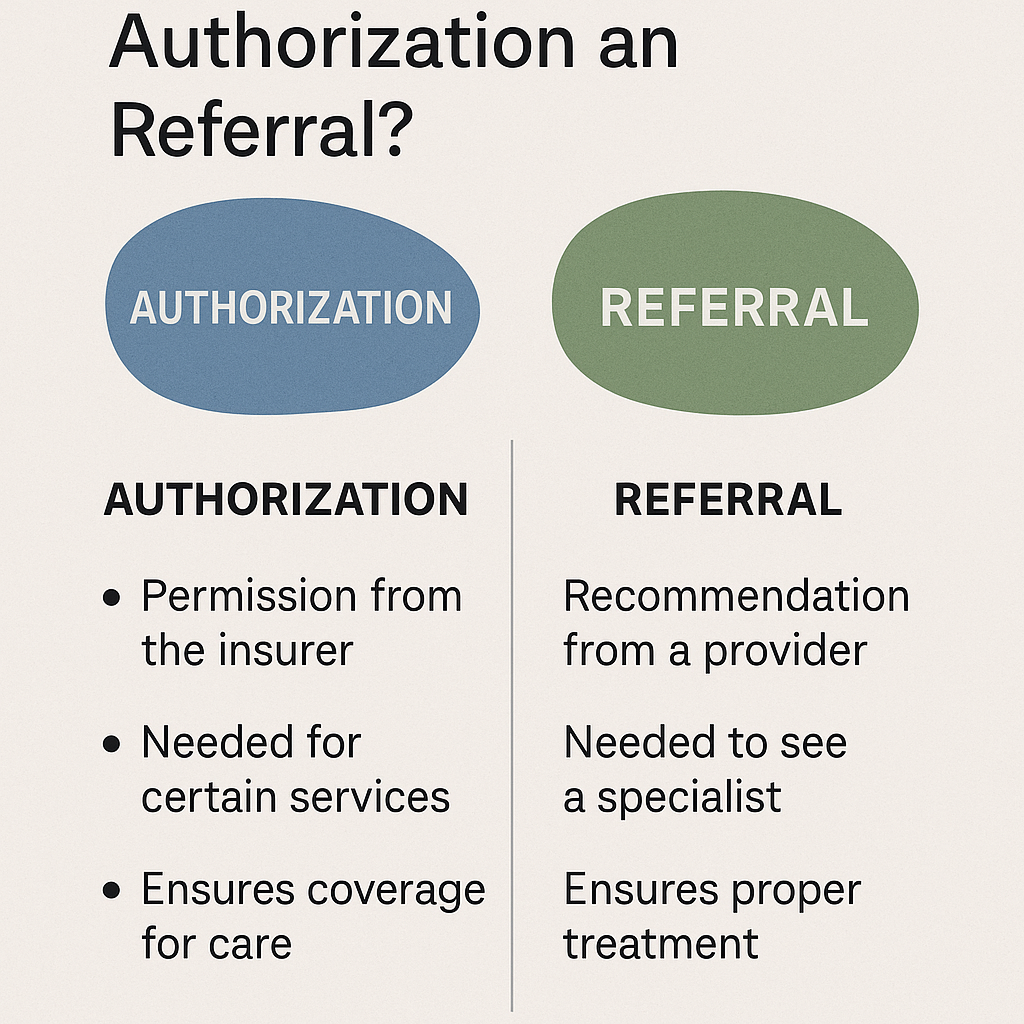
In medical billing, authorization and referral serve different purposes, though both are crucial for insurance coverage and patient care. Simply put, authorization is permission from the insurance company for a service, while a referral is a recommendation from a primary care provider (PCP) to see a specialist. Let’s break down the details to help you understand how they work.
Understanding Authorization: Insurance Pre-Approval
Authorization means the insurer approves a medical service before you get it.
Many health plans require prior authorization to cover specific treatments, procedures, or medications. The goal is to confirm the service is medically necessary.
Key points:
- Comes from the insurance company
- Needed before certain services (e.g., MRIs, surgeries)
- Helps control costs and prevent unnecessary care
- Doesn’t guarantee payment but increases likelihood
What Is a Referral? A PCP’s Recommendation
A referral is when your primary care provider sends you to a specialist.
Referrals are usually required by Health Maintenance Organization (HMO) plans. They help coordinate care within a network.
Key points:
- Comes from a doctor, not the insurer
- Directs patients to a specialist
- Ensures care continuity and keeps costs down
- Required mostly by HMO-type insurance plans
Side-by-Side Comparison Chart: Authorization vs. Referral
| Feature | Authorization | Referral |
|---|---|---|
| Who Issues It? | Insurance Company | Primary Care Provider (PCP) |
| When Needed? | Before high-cost services | Before visiting a specialist |
| Focus | Cost control, medical necessity | Care coordination |
| Required by | PPOs, HMOs, and other plans | Mostly HMOs |
| Affects Payment? | Yes, without it insurance may deny claim | Yes, services may not be covered |
| Examples | MRI, surgery, inpatient care | Dermatologist, cardiologist visit |
Why Do Insurance Plans Require These?
Insurance companies use authorization and referral systems to manage care, reduce unnecessary costs, and ensure that patients get the right treatments.
AI-driven insight: Plans with stricter networks like HMOs rely more on referrals to keep care in-network, while PPOs may need more authorizations for costly services.
Benefits include:
- Controlling healthcare costs
- Avoiding redundant tests
- Promoting care from approved providers
Human Tip: Always call your insurance provider or check your online portal before scheduling care to avoid claim denials.
Visual Aid: Flow Chart of the Process
Referral and Authorization Workflow
- Patient sees PCP → PCP identifies need for specialist → Referral created
- Specialist appointment scheduled → If service requires pre-approval → Authorization requested
- Insurance reviews request → Approves or denies service → Patient receives care
Key Takeaways
- Authorization = Insurance company permission
- Referral = Doctor’s recommendation
- Both are critical in medical billing and impact whether insurance pays
- Know your plan type (HMO vs PPO) to avoid out-of-pocket surprises
FAQs
1. Can you get an authorization without a referral?
Yes, some services only need authorization from the insurance company. However, certain plans require a referral first.
2. What happens if you don’t get authorization?
The claim may be denied, and you might have to pay the full cost out-of-pocket.
3. Is a referral a type of authorization?
No. A referral is from a provider; authorization is from your insurance. They serve different but related roles in healthcare.