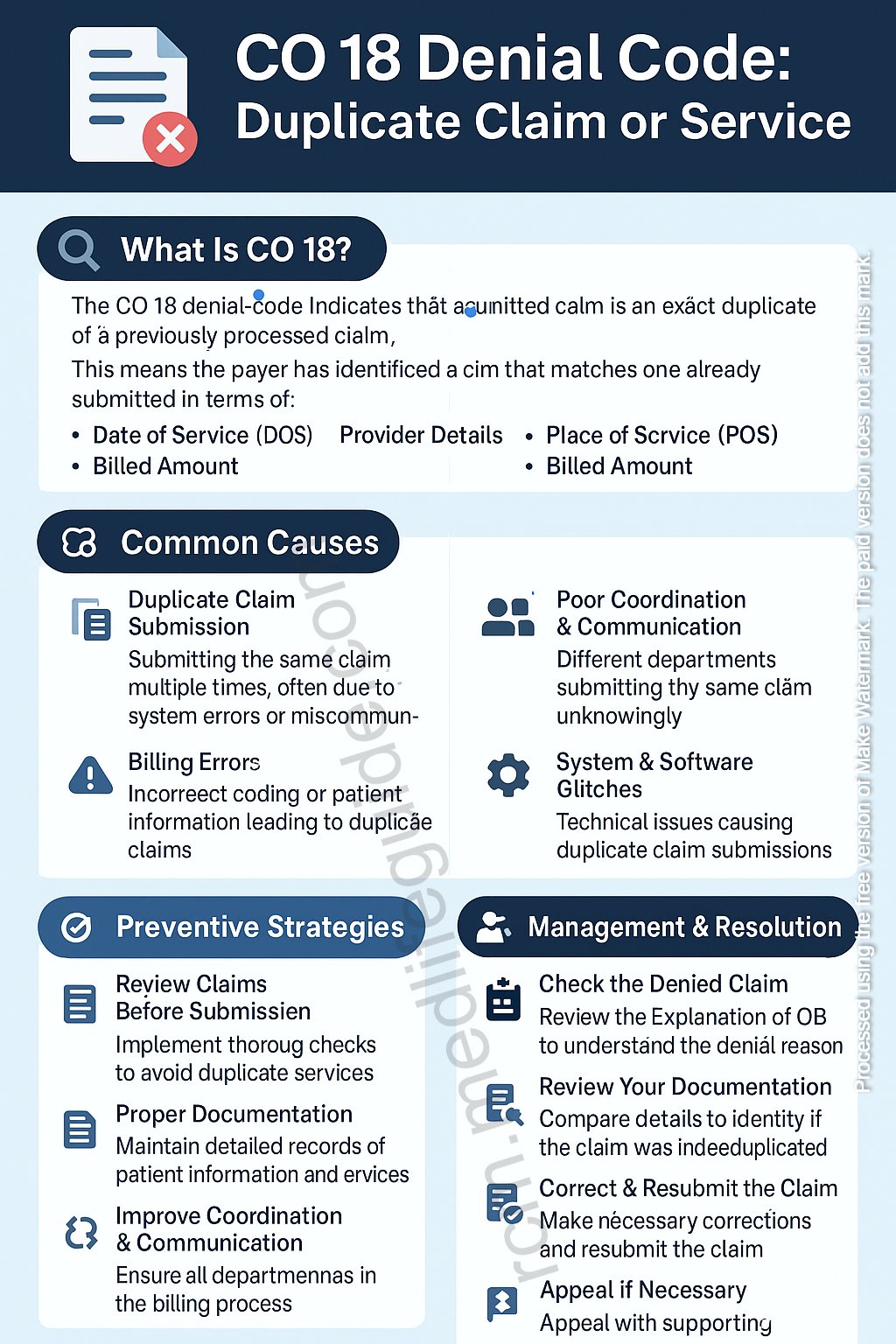
Denial Code 18 signifies that the insurance payer has rejected the claim because it appears to be a duplicate submission. This occurs when a provider submits the same claim multiple times, whether intentionally or unintentionally, before the original claim has been fully processed.
Common Causes of Denial Code 18
Several factors contribute to Denial Code 18, including:
- Unintentional Duplicate Submission
- The claim was mistakenly submitted multiple times due to human error or a system glitch.
- Resubmission Without Proper Follow-Up
- If a provider resubmits a claim without checking the status of the original submission, the payer may flag it as a duplicate.
- Multiple Submissions of the Same Service on Different Dates
- Some procedures are mistakenly billed more than once without proper justification.
- Delayed Payment Leading to Resubmission
- Providers may resend claims assuming the original was lost, but it may still be in processing.
- Lack of Clear Claim Tracking
- If providers or billing teams do not properly track claim submissions, they may unknowingly submit duplicate claims.
How to Fix Denial Code 18
1. Check Claim Status Before Resubmitting
- Use the payer’s online portal or call customer service to verify the status of the original claim before submitting a duplicate.
- Ensure that the first claim was processed correctly or is pending before taking any further action.
2. Compare the Denied Claim with the Original Submission
- Review the claim details, including date of service, CPT codes, provider information, and diagnosis codes, to confirm whether it was truly a duplicate.
- If it was submitted in error, no further action is needed.
3. Identify and Correct Billing Errors
- If the claim was rejected due to missing information rather than being an actual duplicate, correct the errors and resubmit it with proper documentation.
4. Submit an Appeal for Incorrect Denial
- If you determine that the claim was not a duplicate and was wrongly denied, submit an appeal letter along with supporting documents, such as:
- Explanation of Benefits (EOB) showing differences between claims.
- Medical records demonstrating why the service was necessary.
- Any authorization numbers or correspondence supporting claim legitimacy.
5. Use Correct Modifiers to Avoid Duplicate Denials
- In cases where the same service was legitimately provided multiple times, use appropriate modifiers like:
- Modifier 76 (Repeat procedure by same provider)
- Modifier 77 (Repeat procedure by different provider)
- Modifier 59 (Distinct procedural service) when separate and necessary services were performed.
6. Communicate with the Insurance Payer
- If the denial is unclear, reach out to the payer’s representative to clarify why the claim was denied and what actions are needed for reconsideration.
7. Resubmit Only If Necessary
- If the claim is truly a duplicate, do not resubmit it.
- If resubmission is necessary due to an error, ensure it includes the necessary corrections and justification.
How to Prevent Denial Code 18 in the Future
Preventing duplicate claim denials requires a structured and efficient billing process. Here are some best practices:
1. Implement a Robust Claim Tracking System
- Use billing software that logs each claim submission and status update.
- Avoid submitting claims without checking their current status in the system.
2. Educate Billing Staff on Claim Submission Protocols
- Train billing teams on proper submission procedures, including checking claim status before resubmitting.
- Establish guidelines for when and how to follow up on claims.
3. Monitor Payer Processing Timeframes
- Understand the average processing time for each insurance payer.
- Set up internal timelines for following up on unpaid claims instead of blindly resubmitting them.
4. Use Clearinghouse Reports Effectively
- Clearinghouses provide reports on claim submissions, including possible duplicates.
- Review these reports carefully before taking further action.
5. Set Up Alerts for Duplicate Claims
- Some billing systems allow for alerts when a claim with the same details has already been submitted.
- Activate these alerts to avoid unnecessary duplicate submissions.
6. Ensure Proper Use of Modifiers
- When submitting multiple similar claims for the same patient, ensure correct modifier usage to differentiate services.
7. Regularly Audit Billing Practices
- Conduct periodic audits to identify trends in duplicate claim denials.
- Use audit results to implement corrective measures and improve billing accuracy.
Conclusion
Denial Code 18 is a common issue in medical billing but can be effectively managed and prevented with the right strategies. By implementing proper claim tracking, staff education, and thorough review processes, providers can reduce the likelihood of duplicate denials. If a claim is denied due to this reason, promptly investigating, correcting any errors, and using appropriate modifiers will help resolve the issue efficiently. Prevention is always better than correction, and by refining billing processes, healthcare providers can ensure a smoother revenue cycle and fewer claim denials.