Retro authorization has become a quiet but significant drag on many organizations’ revenue cycles. What often starts as a one-off “cleanup” activity can quickly turn into a recurring, costly workaround—masking deeper process issues that eat away at margins and staff capacity.
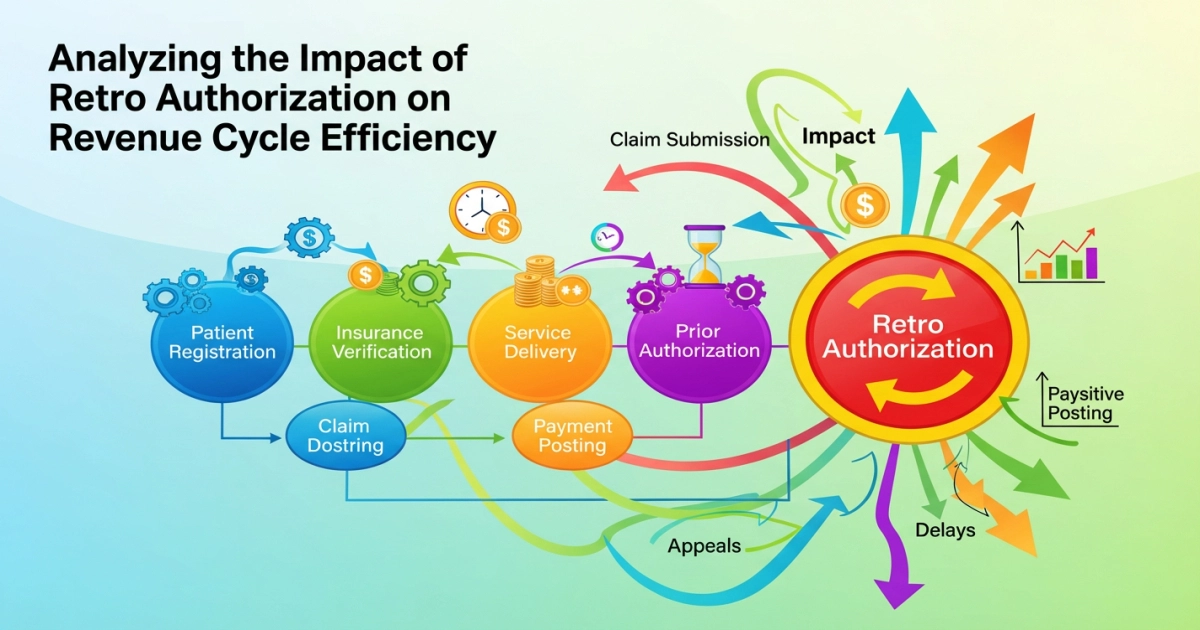
This article analyzes the impact of retro authorization on revenue cycle efficiency, explains why it happens, and outlines practical strategies—process, analytics, and technology—to reduce reliance on retro auth while strengthening overall revenue performance.
What Is Retro Authorization in Healthcare?
Retro authorization (retroactive authorization) is the process of obtaining payer approval for a service after it has already been rendered.
It usually arises when:
- Prior authorization was required but not obtained in advance.
- The patient’s coverage status or plan information was updated after service.
- The service was provided in an emergent or urgent situation where pre-service authorization wasn’t feasible.
Retro authorization is a subset of retroactive authorization revenue cycle management activities and is typically managed by patient access or patient financial services teams, often in coordination with clinical staff.
Retro Authorization vs. Prior Authorization
- Prior authorization
- Approval is obtained before the service.
- Is a standard part of healthcare billing authorization processes.
- If handled properly, it significantly reduces authorization-related denials.
- Retro authorization
- Approval is sought after the service.
- Often viewed as an exception process or damage-control step.
- Carries higher risk of denial and is more labor-intensive.
Reliance on retro authorization is a symptom of front-end breakdowns. An efficient revenue cycle seeks to minimize scenarios where retro auth is needed.
How Retro Authorization Affects Revenue Cycle Efficiency
The medical claims retro authorization impact reaches across the financial, operational, and patient-experience dimensions of the revenue cycle.
1. Financial Impact
- Higher denial risk
- Many payers limit retro auth to narrow circumstances (e.g., emergencies, retro enrollment).
- Claims submitted without required authorization may initially deny. Even with retro auth attempts, approval is far from guaranteed.
- Increased write-offs and underpayments
- When retro auth is denied or only partially approved, organizations may:
- Write off balances as contractual or administrative losses.
- Pursue self-pay from patients who were expecting covered services—often with low yield.
- When retro auth is denied or only partially approved, organizations may:
- Delayed cash flow
- Claims pending retro authorization typically sit in hold queues.
- Additional cycles of submission, denial, retro auth request, and appeal extend days in A/R and hurt cash predictability.
- Higher cost to collect
- Retro auth requires:
- Manual chart review
- Compilation of clinical justification
- Payer calls or portal submissions
- All of this activity occurs after the cost of care has already been incurred, increasing per-claim administrative costs.
- Retro auth requires:
2. Operational Impact & Rework
- Increased rework for staff
- Patient access, PFS, and clinical teams must retroactively:
- Verify benefits
- Gather clinical documentation
- Submit requests and follow up with payers
- These tasks often distract from proactive, pre-service work that prevents issues in the first place.
- Patient access, PFS, and clinical teams must retroactively:
- Fragmented communication
- Retro auth cases frequently expose breakdowns between:
- Scheduling and registration
- Clinical ordering providers and utilization review
- Revenue integrity and billing
- Work tends to happen via ad hoc emails and calls, reducing process consistency.
- Retro auth cases frequently expose breakdowns between:
- Lower staff morale
- Continual firefighting—chasing retro authorizations—creates frustration and burnout.
- Staff feel they are “fixing avoidable mistakes” rather than improving the system.
3. Patient Experience and Satisfaction
- Surprise billing risk
- When authorization is not obtained in advance and retro auth is denied, patients may be:
- Billed unexpectedly
- Forced into payment plans or financial hardship
- This undermines trust and can trigger complaints or formal grievances.
- When authorization is not obtained in advance and retro auth is denied, patients may be:
- Delays in scheduled care
- If retro authorization is discovered before billing but after scheduling, organizations may:
- Reschedule services to secure prior auth
- Delay procedures, frustrating patients and providers.
- If retro authorization is discovered before billing but after scheduling, organizations may:
- Perceived disorganization
- Patients interacting multiple times with patient financial services authorization teams—before and after services—often perceive the organization as disorganized, even when clinical quality is high.
Root Causes: Why Retro Authorization Happens
Retro authorization is rarely just a payer problem. It usually reflects internal issues across front-end, mid-cycle, and back-end processes.
1. Front-End Gaps (Scheduling & Registration)
- Incomplete or inaccurate insurance information
- Outdated coverage details
- Incorrect plan selection or benefit product
- Inadequate authorization screening
- Schedulers or registrars may not:
- Have up-to-date payer rules at their fingertips
- Recognize when services require authorization
- Schedulers or registrars may not:
- Lack of standardized workflows
- No consistent checklist to triage which cases need auth by service, payer, and site of care.
2. Clinical Workflow & Documentation Challenges
- Late or incomplete orders
- Orders may not clearly specify diagnosis, medical necessity, or exact procedures, making proactive authorization difficult.
- Unplanned services added on the day of care
- Additional procedures (e.g., imaging, interventions) may be ordered on the fly, bypassing prior auth workflows.
- Communication disconnects
- Providers may assume authorization is “handled,” but front-end teams lack visibility into changes in clinical plans.
3. Payer Policy Complexity
- Frequent changes in authorization requirements
- Payers revise lists of services requiring auth, approval criteria, and time windows for retro auth.
- Narrow retro auth windows and criteria
- Some payers:
- Only allow retro auth within a short time after service
- Restrict it to emergent scenarios or retroactive enrollment.
- Some payers:
- Inconsistent application of rules
- Variation among payer reps, portals, and written policies leads to confusion and extra administrative effort.
Measuring the Problem: Analytics & KPIs
To manage retro authorization, you must measure it. This is where healthcare revenue cycle analytics becomes essential.
Key Metrics for Retro Authorization
- Percentage of Claims Requiring Retro Authorization
- Numerator: Claims where retro auth work was performed.
- Denominator: Total claims or total claims for services prone to prior auth.
- Goal: Trend down over time; set realistic targets by department.
- Authorization-Related Denial Rate
- Denials with reason codes tied to:
- Missing/invalid authorization
- Lack of prior approval
- Break down by:
- Payer
- Service line
- Site of care
- Use this as part of authorization denial management in healthcare dashboards.
- Denials with reason codes tied to:
- Average Days to Obtain Retro Authorization
- Time from service date to:
- Retro auth approval OR
- Final denial.
- Helps quantify impact on A/R and cash flow.
- Time from service date to:
- Retro Authorization Recovery Rate
- Percentage of initially unauthorized cases that:
- Receive retro auth AND
- Are ultimately paid as expected.
- Highlighted by payer and service category.
- Percentage of initially unauthorized cases that:
- Staff Time per Retro Auth Case (if measurable)
- Time-tracking or sampling to estimate:
- Labor cost
- Opportunity cost vs proactive work.
- Time-tracking or sampling to estimate:
Using Analytics to Drive Action
- Rank payers and service lines by retro auth volume and denial impact.
- Identify root cause categories (e.g., registration errors, order changes, scheduling of non-contracted services).
- Share actionable dashboards with:
- Patient access leadership
- Clinical leadership
- Denial management teams
Strategies for Revenue Cycle Efficiency Optimization
With data in hand, you can design targeted interventions for revenue cycle efficiency optimization centered on preventing retro auth in the first place.
1. Strengthen Healthcare Billing Authorization Processes
- Standardized pre-service screening
- Build and maintain a service-by-payer matrix of authorization requirements.
- Integrate this matrix into scheduling and registration workflows.
- Pre-registration and insurance verification
- Verify benefits and plan details several days before scheduled services.
- Confirm whether:
- Authorization is needed
- A referral is required
- The provider or facility is in-network.
- Clear ownership and SLAs
- Define who is responsible for:
- Identifying cases needing auth
- Obtaining authorization
- Communicating status to clinical and scheduling teams.
- Set service-level expectations for turnaround.
- Define who is responsible for:
2. Robust Authorization Denial Management in Healthcare
- Dedicated denial queues and worklists
- Route authorization-related denials to specialized staff trained in:
- Payer policies
- Efficient submission of retro auth and appeals.
- Route authorization-related denials to specialized staff trained in:
- Root cause feedback loops
- For each denial, capture the primary cause (not just the payer’s reason code).
- Feed trends back to:
- Registration training programs
- Clinical service leaders
- Ordering providers.
- Standardized appeal templates and escalation paths
- Use templates with clear:
- Clinical justification
- References to payer policies
- Implement escalation paths for recurring or systemic payer issues.
- Use templates with clear:
3. Cross-Functional Collaboration
- Link patient access, utilization review, and clinical teams
- Regular meetings on:
- High-denial service lines
- Changes in payer policies
- Complex cases with recurring retro auth needs.
- Regular meetings on:
- Engage physicians and APPs
- Educate ordering providers on:
- Services frequently requiring auth
- Importance of complete orders and documentation.
- Educate ordering providers on:
- Partner with payers where feasible
- Request clarification on:
- Retro auth policies
- Electronic prior auth options
- Explore delegated or streamlined arrangements for high-volume services.
- Request clarification on:
Retro Authorization Workflow Automation & Technology
Technology can significantly reduce manual effort and error-prone steps in both prior and retro auth.
1. Opportunities for Retro Authorization Workflow Automation
Automation can help:
- Identify at-risk encounters early
- Flag scheduled cases missing required auth well before service date.
- Pre-populate retro auth requests
- Pull clinical and demographic data from the EHR into payer-specific forms.
- Automate status checks
- Use bots or integrations to:
- Check payer portals
- Update statuses in your RCM or EHR.
- Use bots or integrations to:
These capabilities are increasingly bundled into healthcare reimbursement authorization systems and broader RCM platforms.
2. Role of Healthcare Reimbursement Authorization Systems
Modern systems can:
- Maintain payer rule libraries that alert staff when prior auth is required.
- Provide work queues specifically for:
- New auth requests
- Retro auth follow-ups
- Denial appeals.
- Integrate with scheduling, registration, and clinical documentation systems to reduce duplicate data entry.
When selecting or optimizing such systems, evaluate:
- Breadth and accuracy of payer rules (and how often they’re updated).
- Depth of integration with your existing EHR and billing tools.
- Support for both standard prior auth and exceptional retro auth workflows.
Compliance, Risk, and Retro Authorization Regulations
Retro authorization is not just a financial concern—it’s a compliance and regulatory issue.
1. Retro Authorization Compliance and Regulations
Key themes to manage:
- Payer contract compliance
- Many contracts specify:
- Circumstances under which retro auth is allowed
- Documentation requirements
- Timeframes for requests.
- Many contracts specify:
- Emergent vs non-emergent care
- Regulations and payer policies often distinguish:
- Genuine emergencies (where retro auth is more readily granted)
- Elective or scheduled procedures (where failure to obtain prior auth may not be excusable).
- Regulations and payer policies often distinguish:
- Medical necessity and documentation
- Retro auth reviews may be more stringent, requiring:
- Thorough clinical justification
- Clear alignment with medical necessity criteria.
- Retro auth reviews may be more stringent, requiring:
2. Audit and Refund Risk
Heavy reliance on retro authorization can:
- Increase exposure during payer audits and internal compliance reviews.
- Trigger takebacks if payers determine:
- Auth should have been obtained in advance
- Retro auth was granted outside policy.
Mitigation steps:
- Maintain a clear audit trail for each retro auth case:
- Rationale
- Documentation submitted
- Payer communications.
- Periodically review retro auth cases for:
- Pattern deviations from contracts
- Any improper billing practices.
Implementation Roadmap: From Insight to Action
To reduce reliance on retro auth while improving revenue cycle efficiency, consider a phased approach:
Phase 1: Assess and Baseline
- Quantify:
- Volume of retro auth cases
- Related denials and financial impact
- Days in A/R tied to authorization issues.
- Map existing workflows:
- Front-end authorization checks
- Retro auth handling steps
- Escalations and exception paths.
Phase 2: Design Improvements
- Redesign front-end workflows:
- Standardize checklists and scripts for scheduling and registration.
- Establish pre-registration timelines and responsibilities.
- Enhance denial management:
- Build dedicated authorization denial worklists.
- Implement root cause coding and monthly trend reviews.
- Address policy and education:
- Update policies to:
- Minimize scheduling without required auth (except emergencies).
- Educate staff and providers on new processes and payer rules.
- Update policies to:
Phase 3: Enable with Technology
- Optimize existing tools or implement new authorization systems:
- Integrate payer rule libraries and alerts.
- Configure work queues for both prior and retro auth.
- Explore automation:
- Automate benefits verification and auth status checks.
- Use bots or integrations for high-volume payer portals.
Phase 4: Monitor, Refine, and Sustain
- Track KPIs:
- Retro auth volume and rate
- Authorization-related denials
- Days in A/R for affected claims.
- Conduct regular cross-functional reviews:
- Share dashboards with clinical and operational leaders.
- Adjust workflows as payer policies and service lines evolve.
Frequently Asked Questions (FAQ)
1. What is retro authorization in healthcare?
Retro authorization is the process of obtaining payer approval for a service after it has already been provided. It is typically used when prior authorization was missed or when services were delivered in an emergency.
2. How does retro authorization affect the revenue cycle?
Retro authorization can:
- Increase denial rates
- Delay claim payment and increase days in A/R
- Add administrative costs through rework
- Create compliance and audit risks if not managed properly.
3. Is retro authorization always allowed by payers?
No. Many payers:
- Limit retro authorization to specific situations (e.g., emergencies, retro enrollments).
- Impose strict time windows and documentation requirements.
Organizations should understand each payer’s rules and monitor adherence.
4. How can we reduce retro authorization in our organization?
Focus on:
- Strengthening front-end authorization workflows
- Using healthcare revenue cycle analytics to identify root causes
- Training staff on payer rules
- Leveraging authorization systems and automation
- Establishing strong denial management and feedback loops.
5. What role does automation play in retro authorization workflows?
Automation can:
- Flag encounters missing required auth
- Pre-populate request forms with EHR data
- Automatically check payer portals for auth status.
While it cannot replace all judgment, retro authorization workflow automation can significantly reduce manual burden and error.
Conclusion & Key Takeaways
Retro authorization may feel like a necessary safety net, but overreliance on it is a clear warning sign of inefficiencies in the revenue cycle.
By:
- Precisely measuring medical claims retro authorization impact
- Strengthening healthcare billing authorization processes at the front end
- Investing in authorization denial management in healthcare
- Leveraging healthcare reimbursement authorization systems and targeted automation
- Maintaining vigilance over retro authorization compliance and regulations
organizations can protect revenue, streamline operations, and provide a better experience for patients and staff alike.
In the end, the most efficient retro authorization is the one you rarely need—because your processes, analytics, and technology prevent problems before they start.